Principle Member
From R4531
Dependant Member
From R3562
Child Dependant
From R1809
Essential Priority
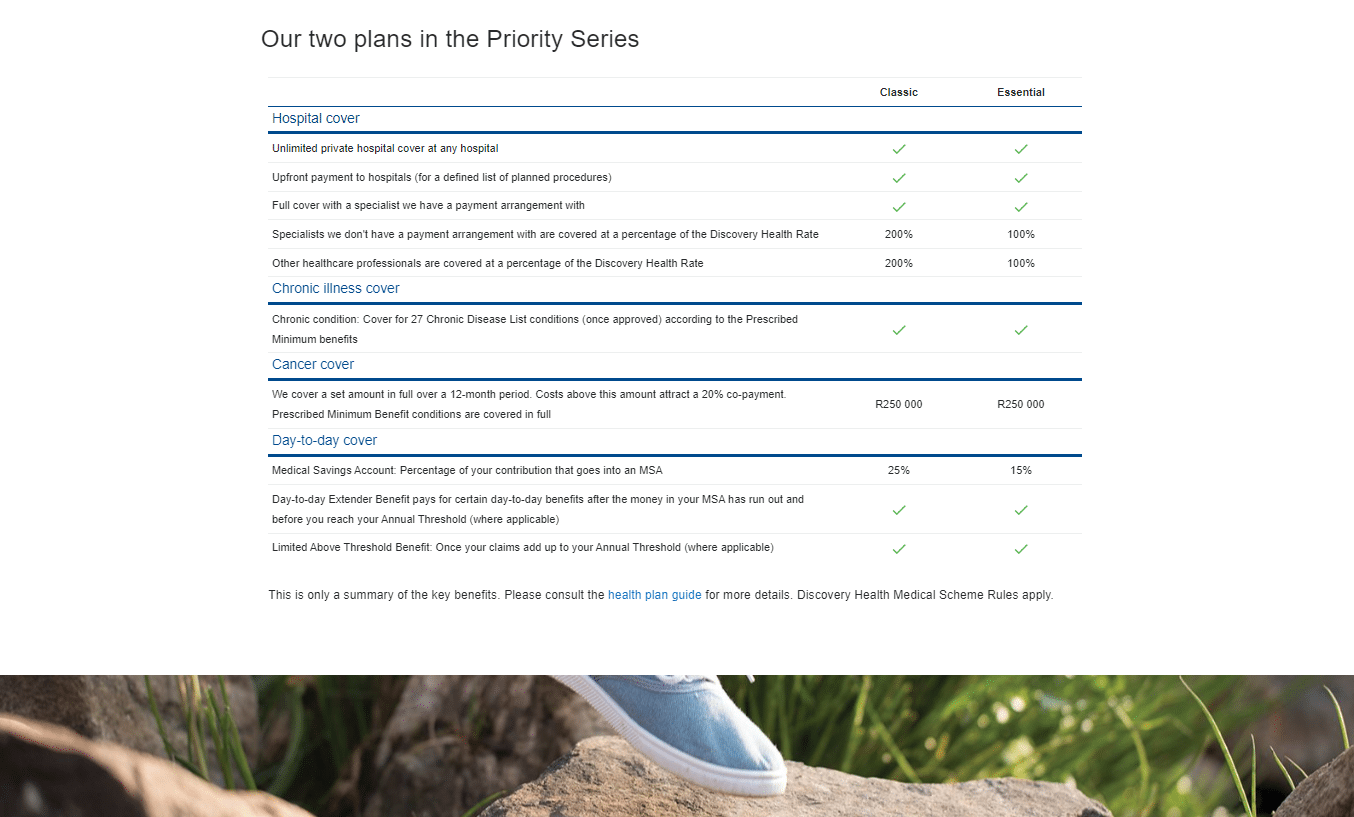
The Essential Priority plan is a good option for those who prioritize affordability over a wide range of benefits, it provides comprehensive and flexible coverage for medical expenses,
★★★★★ 4.5/5
Chronic Cover:
Day-to-Day:
Preventative Care:
Cancer Cover:
Hospitalisation:
Maternity Benefits:
The Essential Priority plan is a good option for those who prioritize affordability over a wide range of benefits, it provides comprehensive and flexible coverage for medical expenses,
Tax Deductible:
Travel Cover:

Essential Priority
The Essential Priority plan is a good option for those who prioritize affordability over a wide range of benefits, it provides comprehensive and flexible coverage for medical expenses,
★★★★★ 4/5
Principle Member
From R4531
Dependant Member
From R3562
Child Dependant
From R1809
Chronic Cover:
Day-to-Day:
Preventative Care:
Cancer Cover:
Hospitalisation:
Maternity Benefits:
The Essential Priority plan is a good option for those who prioritize affordability over a wide range of benefits, it provides comprehensive and flexible coverage for medical expenses,
Tax Deductible:
Travel Cover: