Principle Member
From R1102
Dependant Member
From R1102
Child Dependant
From R664
KeyCare Start Regional
The KeyCare Start Regional plan focuses on providing basic healthcare coverage at an affordable price, with services and facilities within a specific geographic region.
★★★★★ 4.5/5
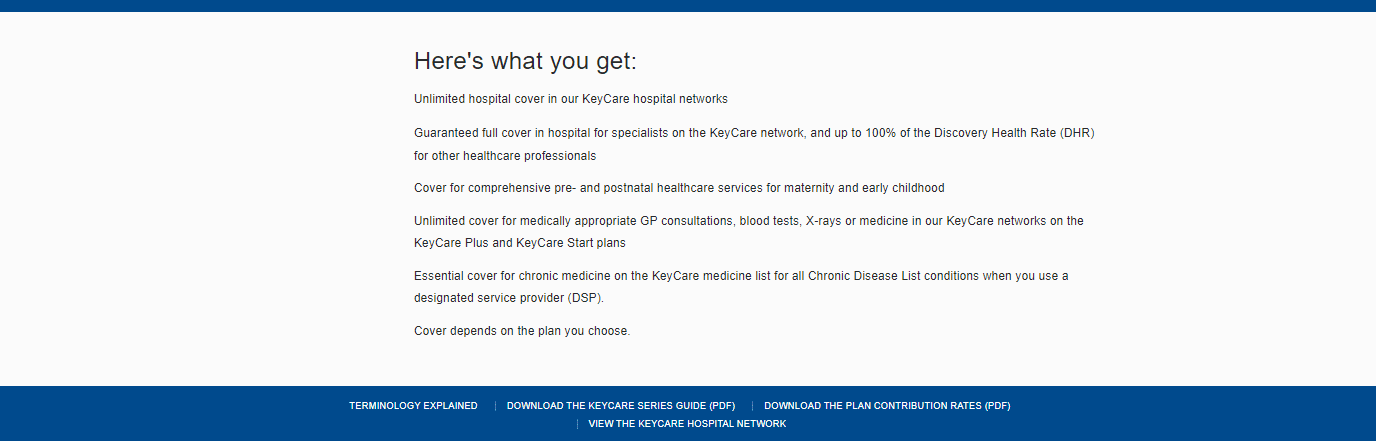
Chronic Cover:
Day-to-Day:
Preventative Care:
Cancer Cover:
Hospitalisation:
Maternity Benefits:
The KeyCare Start Regional plan focuses on providing basic healthcare coverage at an affordable price, with services and facilities within a specific geographic region.
Tax Deductible:
Travel Cover:

KeyCare Start Regional
The KeyCare Start Regional plan focuses on providing basic healthcare coverage at an affordable price, with services and facilities within a specific geographic region.
★★★★★ 4/5
Principle Member
From R1102
Dependant Member
From R1102
Child Dependant
From R664
Chronic Cover:
Day-to-Day:
Preventative Care:
Cancer Cover:
Hospitalisation:
Maternity Benefits:
The KeyCare Start Regional plan focuses on providing basic healthcare coverage at an affordable price, with services and facilities within a specific geographic region.
Tax Deductible:
Travel Cover: