Principle Member
From R2714
Dependant Member
From R2037
Child Dependant
From R1078
Coastal Core
The Coastal Core plan offers various benefits such as Discovery Health Connected Care, pathology, and radiology services, as well as in and out-of-hospital cover.
★★★★★ 4.5/5
Chronic Cover:
Day-to-Day:
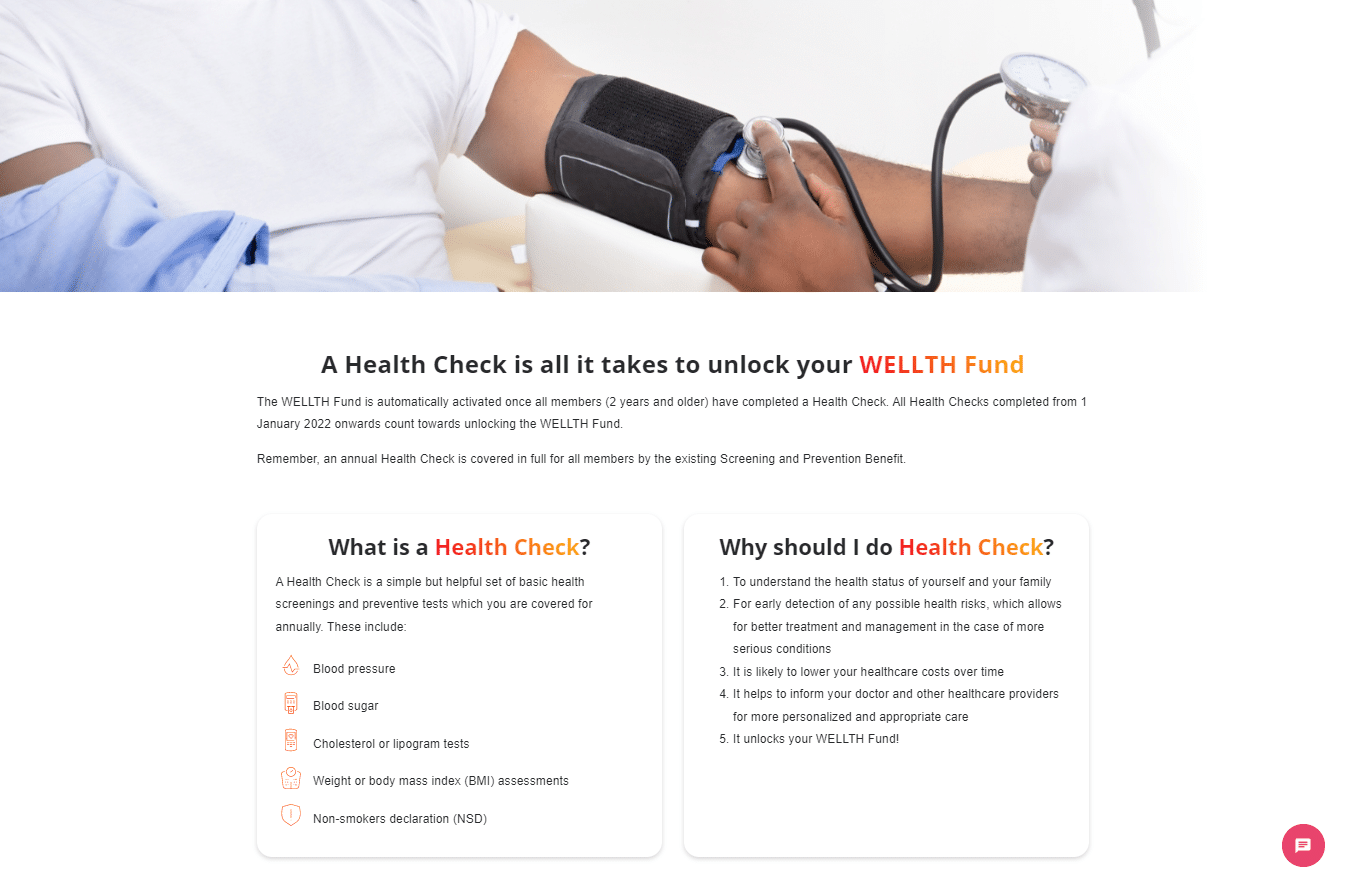
Preventative Care:
Cancer Cover:
Hospitalisation:
Maternity Benefits:
The Coastal Core plan offers various benefits such as Discovery Health Connected Care, pathology, and radiology services, as well as in and out-of-hospital cover.
Tax Deductible:
Travel Cover:

Coastal Core
The Coastal Core plan offers various benefits such as Discovery Health Connected Care, pathology, and radiology services, as well as in and out-of-hospital cover.
★★★★★ 4/5
Principle Member
From R2714
Dependant Member
From R2037
Child Dependant
From R1078
Chronic Cover:
Day-to-Day:
Preventative Care:
Cancer Cover:
Hospitalisation:
Maternity Benefits:
The Coastal Core plan offers various benefits such as Discovery Health Connected Care, pathology, and radiology services, as well as in and out-of-hospital cover.
Tax Deductible:
Travel Cover: