
5 Best Medical Aid with Immediate Cover (No Waiting Period)
Should you decide to change between medical aids, the new medical aid may impose a three-month general waiting period, even when you did belong to a medical scheme for more than 24 months and did not have a break of more than 90 days.
The reason for this is purely to safeguard medical aids against anti-selection (members doing “scheme-hopping” for specific benefits, make use of them, and then resign)
We tested them side by side and verified their medical aid plans.
This is a complete guide to the best medical aid with immediate cover in South Africa.
In this in-depth guide you’ll learn:
- What is a Medical Aid?
- Which medical aid is affordable in South Africa?
- How to choose the best affordable medical aid for your needs?
- How to compare medical aids against each other?
- Which Medical Aid is Best in South Africa?
- How do you choose the best medical aid for your family?
So if you’re ready to go “all in” with the best medical aid with Immediate Cover in South Africa, this guide is for you.
Let’s dive right in…
5 Best medical aid with immediate cover (no waiting period)
| 🩺 Medical Aid | ✔️ Provides Cover Immediately? | ⚕️ Plan Offered | 👉 Sign Up |
| 1. Bonitas | Yes | Edge Plans | 👉 Apply Now |
| 2. Discovery Health | Yes | Discovery KeyCare Plan | 👉 Apply Now |
| 3. Momentum Health | Yes | Evolve Option | 👉 Apply Now |
| 4. BestMed Medical Aid | Yes | flexiFED Savvy | 👉 Apply Now |
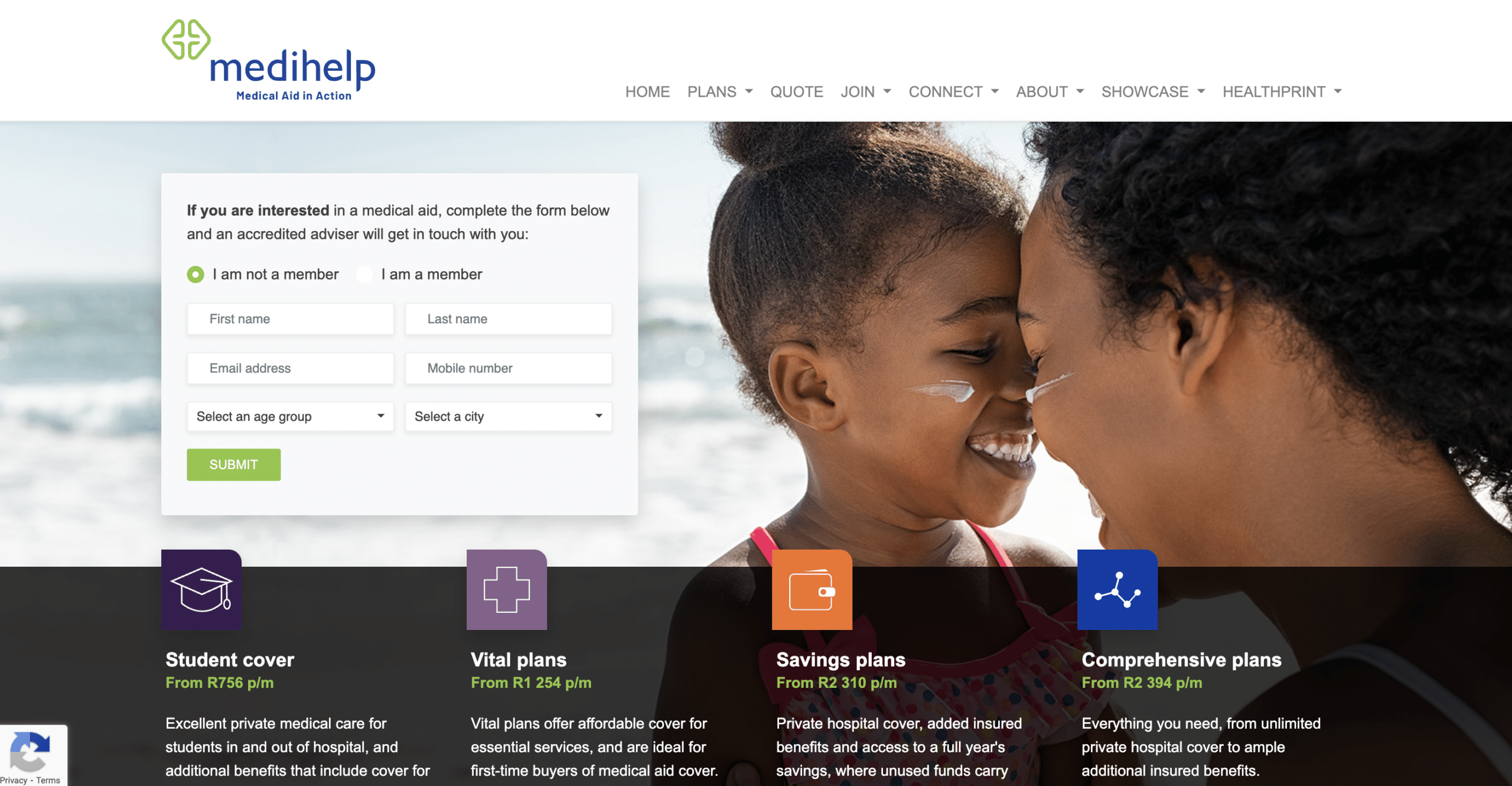
| 5. Medihelp Medical Aid | Yes | Network Plans | 👉 Apply Now |
5 Best Medical Aid With Immediate Cover Summary
- Bonitas – Overall, Best Medical Aid with Immediate Cover in South Africa
- Discovery Health – Best Variety of Benefits
- Momentum Health – Top Hospital Plans with No Yearly Limits
- BestMed Medical Aid – Largest Self-Administered Medical Plans
- Medihelp Medical Aid – Best Customer Service Medical Aid
Understanding immediate cover from medical aid in South Africa

👉 If you are in desperate need of medical care and are in the market for a medical aid scheme, you should be aware that you will likely be subject to a waiting period unless you are fortunate enough to join an employment group that has an exemption.
👉 When it comes to those with pre-existing medical conditions, medical aids typically don’t waive waiting periods.
👉 If a medical aid scheme grants you an exemption from the waiting period, it must grant the same exemption to everyone else in a comparable position. For this reason, all medical aid schemes will impose a waiting period on new members.
Why do medical aids impose a waiting period

👉 When first joining a medical aid, new members may be confused as to why there is a waiting period before they can make a claim.
👉 Considering that a medical aid manages a pool of funds to cover all members’ claims and considering that a single claim can cost tens of thousands, if not hundreds of thousands of rands, waiting periods are a sensible measure.
👉 Waiting periods exist primarily to guarantee that people do not just join a medical aid when they require expensive medical treatment and then resign, dramatically reducing the pool of cash available for all members’ requirements.
👉 A waiting period is thus a set period of time during which members may be ineligible to claim while paying monthly contributions.
👉 This protects and is in the best interests of all members, as well as supporting the medical aid’s financial stability.
👉 However, when a child dependant is born to an existing member of a medical aid, the new born is exempt from waiting periods.
👉 Unless the individual has never contributed to a medical scheme previously or has had a lapse in membership of more than 90 days, waiting periods normally exclude life-threatening crises and specified minimum benefits (PMBs).
👉 In some situations, a new member who joins the medical aid with a pre-existing health condition may be ineligible to claim treatment for that condition for up to 12 months.
👉 When a member leaves a different medical scheme after less than or up to 24 months, they may face a condition-specific waiting time, including pregnancy.
👉 If the previous membership lasted more than 24 months and there was no 90-day break, a three-month general waiting period may apply. Because pregnancy is a PMB, the same restrictions apply to waiting periods.
👉 It is critical to understand what you are insured for and which waiting periods apply to you from the start.
👉 Remember that, depending on the plan you select, your medical aid may impose restrictions on hospitalisation. As a result, it is critical that you ensure that the benefits supplied will suit your individual needs as well as those of your dependents.
READ more about the comparisons between Medical Aid and a Hospital Plan
Special cases in which waiting periods may not apply

👉 There are four possible cases in which a waiting period may not apply when joining a medical aid scheme:
➡️ You are changing plans within the same scheme. This is usually only allowed once a year.
➡️ You are changing from medical aid compulsory due to a change in work. Only applicable should you change from a closed medical aid eg. Bankmed, and have to move to an open medical aid since you are no longer eligible to belong to eg. Bankmed as a private member.
➡️ You work for a company that has an agreement with the medical aid to waive all waiting periods for its employees and dependents.
➡️ In some situations, your new medical aid may waive waiting periods based on their own discretion.
1. Bonitas

Overview
👉 Bonitas has been in business for nearly 40 years, which has given them a rich tradition and a thorough understanding of the South African private healthcare sector.
👉 As a result, whether it’s keeping a finger on the technological pulse, managing your care so lifestyle diseases are identified before they become chronic, or negotiating better rates for you, its team of experts is always looking for new ways to ensure that members receive affordable, high-quality healthcare.
👉 If you are one of more than 700,000 beneficiaries, you can benefit from Bonitas’ lower pricing and dependable service providers to keep you healthy while keeping healthcare costs under control.
👉 Bonitas’ wide range of options ensures that you and your family will discover the best fit for your specific needs. The plans are intended to be simple to use while simultaneously providing the best possible benefits. Bonitas is available if you are a young adult seeking your first medical aid, a young family or an older member with more comprehensive medical needs.
👉 Bonitas has strong main indicators of fiscal health, stable finances, and more than R6 billion in reserves.
👉 One of Bonitas’ strategy pillars is connecting with consumers since it allows them to be member-centric and devoted to serving their best interests.
Bonitas Medical Aid Plans
👉 Bonitas provides a wide range of plans. The plans are simple to comprehend and apply, allowing new members to get the most out of their advantages.
Edge Plans
👉 This category provides access to daily benefits such as unlimited GP appointments, virtual care layers, dental and optical consultations, a private hospital network, and more. The BonStart plan is designed for economically active singles living in bigger metro areas who are driven to achieve, and the BonStart Plus plan is geared for young, economically active couples living in larger metro areas who are wanting to grow their family.
Traditional Plans
👉 Traditional plans are appropriate for those who are more settled and financially independent. They include an overall daily limit, as well as sub-limits for GP and specialist appointments, acute and over-the-counter medication, X-rays and blood tests, and other out-of-hospital medical expenses. Standard, Standard Select, Primary, and Primary Select plans are available.
👉 This standard option provides good day-to-day benefits and full hospital coverage, whereas the Select plans give limited day-to-day benefits and hospital coverage through a network of quality doctors.
Savings Plans
👉 New members could also consider one of Bonitas’ Saving plans, which provide a specific amount that can be used for out-of-hospital expenses such as doctor visits, optometrist, and dentistry. They also cover you in the hospital and provide additional benefits for maternity, wellness, and preventative care.
👉 BonFit Select, BonSave, BonComplete, BonClassic, and BonComprehensive are the available options.
👉 This savings option provides enough resources to meet medical bills and extensive hospital coverage, with BonComprehensive being a first-rate savings plan that provides abundant savings, an above-the-threshold benefit, and the greatest hospital coverage.
Hospital Plans
👉 Members can also choose hospital plans, which cover them for emergency and planned hospital operations as well as some additional benefits for wellness and preventative care.
👉 These plans include the Hospital Standard, BonEssential, and BonEssential Select, the latter of which uses a quality provider network and provides complete hospital benefits as well as some value-added benefits.
Bonitas Waiting Period Conditions
➡️ 3-Month General Waiting Period If you are a private individual that has not joined as part of your employer group, a 3-month general waiting period will apply. During this period you cannot claim for any benefits.
➡️ Dependants of a deceased member, who are registered with the Scheme as dependants at the time of the member’s death, will be entitled to continued membership of the Scheme without any new restrictions, limitations or waiting periods.
How Much Are Bonitas Medical Aid’s Monthly Premiums?
👉 Bonitas monthly contributions start at R2,287 for a Principal Member, R1,690 for a spouse/adult dependant and R739 per child (max 3) on the BonEssential Hospital Plan and go up to R9,853 for a main member, R9,292 for additional adult, and R2,006 for a child for the BonComprehensive plan that offers abundant savings, an above threshold benefit and extensive hospital cover.
What Is the Waiting Period for Bonitas Medical Aid Benefits?
👉 The minimum general waiting period for Bonitas medical aid is three months for all benefits. Some plans, however, have a waiting period of 12 months, especially regarding a pre-existing condition.
👉 Pregnancy is considered a pre-existing condition; therefore, it is excluded from all benefits for the first 12 months of scheme membership.
How to Claim from Bonitas
👉 You can send in your claim in the following ways:
➡️ Email your claims to [email protected].
➡️ Post your claims to Bonitas Claims Department, PO Box 74, Vereeniging, 1930.
➡️ Submit your claims in person at one of the walk-in centres.
👉 Follow these simple steps to get your claims paid quickly:
➡️ Ensure your banking details are correct for refunds by electronic transfer (EFT) into your bank account
➡️ Make sure that your account and receipt show your name and initials, membership number, treatment date, the name of the patient as shown on your membership card, the amount charged and ICD-10 code.
Bonitas Contact Details
34 Melrose Blvd, Birnam
Johannesburg
2196
Phone for General Queries: 0860002108
Email: [email protected]
Email: [email protected]
READ more about Stratum Benefits Health Insurance
2. Discovery Health
Overview
👉 Discovery Health provides over 20 different options, all of which include unlimited private hospital coverage and a variety of incentives to meet everyone’s needs and financial circumstances.
👉 These options provide access to a variety of benefits, care plans, and services to ensure any young adult receives the greatest medical care when they require it.
👉 According to Discovery, competitor South African medical aids charge an average 14.9% higher in contributions for the same level of coverage, which is a very appealing aspect for young people who may not earn high salaries yet.
👉 You can also join Vitality, the company’s wellness programme, which rewards you for living a healthy lifestyle with gym memberships and other perks. This has an additional monthly cost.
👉 The management of Discovery Health, which is owned by its members, is overseen by an independent Board of Trustees.
👉 It is handled by a different business, Discovery Health (Pty) Ltd, an authorised financial services provider. Discovery Health Medical Scheme is governed by the Medical Schemes Act and the Council for Medical Schemes.
Discovery Health Medical Aid Options
👉 Discovery Health’s options range from the most comprehensive but pricey private healthcare coverage to basic and less expensive options that give cost-effective private healthcare coverage through a large network of providers.
Comprehensive Series
👉 The Comprehensive series of plans offers comprehensive in-hospital and day-to-day coverage, as well as extended chronic medicine coverage and an unlimited Above Threshold Benefit. Because of the relatively expensive premiums, members who are already established in steady work should consider this.
The Discovery Health Comprehensive Series includes the following plans:
- Classic Comprehensive
- Classic Delta Comprehensive
- Classic Smart Comprehensive
- Essential Comprehensive
- Essential Delta Comprehensive
Priority Series
👉 The Priority Series Medical Aid plans are appropriate for young professionals because they provide cost-effective in-hospital coverage, necessary chronic medicine coverage, and day-to-day benefits with a restricted Above Threshold Benefit.
Saver Series
👉 The Saver series is cost-effective, offering in-hospital coverage, necessary chronic medicine coverage, and day-to-day benefits via a Medical Savings Account. Because its rates are reasonable, many young adults join.
The Discovery Health Saver Series offers the following medical aid plans to choose from:
- Discovery Health Classic Saver
- Discovery Health Classic Delta Saver
- Discovery Health Coastal Saver
- Discovery Health Essential Delta Saver
- Discovery Health Essential Saver
Core Series
👉 The Core Series is a low-cost hospital plan that provides members with limited income with unrestricted private hospital coverage and critical chronic medicine coverage. There is no day-to-day coverage included in the benefits.
Smart Series
👉 If members use providers in a designated network, the Smart series of plans provide the most cost-effective in-hospital coverage, necessary chronic medication coverage, and limited day-to-day coverage.
KeyCare Series
👉 Members who are just starting out in their careers may examine the KeyCare Series for basic set of ideas to get their foot in the door. It provides low-cost medical coverage if you use physicians in a specific network for both in-hospital and out-of-hospital care.
Discovery Health Waiting Period Conditions
➡️ Discovery Health applies 12-month condition-specific waiting periods, mandatory three-month general waiting period and late-joiner penalties.
➡️ The Scheme will not consider any underwriting concessions, except for Employer Groups and with specified conditions. Important note: All application forms are valid for a period of 90 days from the date on which a member signs the application form.
➡️ You will not have cover or access to the Prescribed Minimum Benefits during your waiting periods. This includes cover for emergency admissions.
How Much Are Discovery Medical Aid Monthly Premiums?
👉 Monthly premiums start from R1,102 per member for the Keycare Series with medical cover for both in-hospital and out-of-hospital treatment by providers in a specified network and go up to R10,303 per member for the Executive Plan with extensive cover for in-hospital and day-to-day benefits, extended chronic medicine cover, and unlimited Above Threshold Benefit.
What Is the Waiting Period for Discovery Medical Aid’s Benefits?
👉 Discovery Health Medical Scheme’s general waiting period is 3 consecutive months and the condition-specific waiting period is 12 consecutive months.
How to Claim for Discovery Medical Aid Benefits
👉 You can submit a claim fast and easy in the following ways:
➡️ Scan and upload your claims on the website.
➡️ Scan and email your claims to [email protected].
➡️ Use the Discovery app on your smartphone. If the claim has a QR code, scan the QR code or alternatively take a photo of the claim from within the app.
➡️ You can also submit your claims by post.
Discovery Medical Aid Contact Details
PO Box 784262,
Sandton,
2146
Phone: 0860 99 88 77
READ more about The 5 Top Hospital Plans for Infants in South Africa revealed.
3. Momentum Health
Overview
👉 Momentum is one of South Africa’s most effective open medical aids, and it is Administered by one of the country’s largest and most reputable healthcare solutions organisations. Momentum Metropolitan Life Limited, Momentum Health Solutions’ parent business, owns the entire firm.
👉 Momentum Medical Aid is a non-profit open medical scheme that works in accordance with the most recent revised version of the Medical Schemes Act 131 of 1998.
👉 Every year, an Annual General Meeting is held to elect new members to the organization’s Board of Trustees, which includes a large number of persons with extensive experience in medical, accounting, and legal sectors.
Momentum Health Medical Aid Options
👉 Momentum Medical Scheme offers a variety of medical insurance policies and benefits to South Africans, including six medical aid options. These are the options:
Evolve Option
👉 This option provides hospitalisation coverage from the Evolve Network of private hospitals with no yearly limit.
👉 Members who select this option get access to two virtual doctor consultations each month, and any further day-to-day benefits are subject to HealthSaver+.
Custom Option
👉 This option provides full hospital and chronic care coverage from any or affiliated providers to members. They have the option of receiving treatment at any hospital or reducing their contributions by using a particular list of private facilities.
Incentive Option
👉 This top choice is appropriate for members who can afford a higher monthly premium. With this option, members can obtain comprehensive hospital and chronic care coverage from any or all affiliated doctors. Their daily expenses will be paid by a medical savings account funded by 10% of their monthly contributions.
Extender Option
👉 This more expensive option provides extensive hospital care and additional chronic coverage from any or affiliated providers to members who simply need a little extra coverage. 25% of their contributions are directed to a medical savings account, from which all day-to-day expenses are deducted. They will receive the Extended Cover advantage once they have met the Threshold.
Summit Option
👉 This option allows members to obtain limitless private hospital coverage from any provider. A chronic cover is available for 36 diseases, and day-to-day benefits are also covered up to a set sum per beneficiary per year.
Ingwe Option
👉 This is the most economical and accessible choice for members who have just begun their first employment. They can be treated at any hospital, including the Ingwe Network of private hospitals and State hospitals.
Momentum Medical Scheme has a Momentum Multiply Rewards Program
Momentum Health Waiting Period Conditions
➡️ If a 3-month general waiting period is applied, this means that you must wait 3 months from the date that your membership commences before you can claim from your Momentum Medical Scheme benefits.
👉 A 12-month waiting period may also be applied to specific medical conditions. If this waiting period is applied, you will have to wait 12 months from the date your Momentum Medical Aid membership starts before you can claim benefits for the condition.
👉 Should you qualify for the Prescribed Minimum Benefits, you would be eligible to obtain treatment at a State facility, provided that the condition is one that is covered by the Prescribed Minimum Benefits.
How Much Are Momentum Health Monthly Premiums?
👉 Momentum monthly premiums start at R1,687 for the main member on the Evolve Option and go up to R13,573 for the main member on the Summit Option.
Learn more about the medical aid plans that Momentum has to offer:
- ✅ Momentum Summit
- ✅ Momentum Ingwe
- ✅ Momentum Incentive
- ✅ Momentum Extender
- ✅ Momentum Evolve
- ✅ Momentum Custom
What Is the Waiting Period for Momentum Health Benefits?
👉 The general waiting period is 3 months, but since pregnancy is considered a pre-existing condition, it is excluded from all benefits for the first 12 months of scheme membership.
How to Claim Momentum Health Benefits
👉 You can submit a claim in several ways:
➡️ Use the Momentum App
➡️ Use the web chat facility in the bottom left corner.
➡️ Send an email to [email protected] or send normal mail to PO Box 2338, Durban, 4000
👉 To make sure your claim is processed quickly and accurately, including the following information:
➡️ Membership number.
➡️ Principal member’s surname, initials, and first name.
➡️ Patient’s surname, initials, and first name.
➡️ Date of treatment.
➡️ Amount charged.
➡️ ICD–10 code (code to indicate what condition you’ve been diagnosed with), tariff code (product-specific code for procedures and claims), and NAPPI code (a unique identifier for a given ethical, surgical, or consumable product).
➡️ Service provider’s name and practice number.
➡️ Proof of payment if you’ve paid the claim out of your own pocket.
Momentum Health Contact Details
201 Umhlanga Ridge Blvd
Cornubia
Blackburn
PO Box 2338
Durban
READ more about Medshield in comparison with Momentum Medical Scheme
4. BestMed Medical Aid
Overview
👉 BestMed claims to be South Africa’s largest self-administered medical plan and the fourth-largest open medical plan overall.
👉 BestMed has a history of connecting young adult members with a network of healthcare professionals, wellness perks, and cost-effective healthcare coverage options.
👉 The organisation is rather proud of its recent continuous single-digit growth, as well as its 13 well-organized products that cover every potential life stage and financial necessity.
👉 All of its alternatives provide considerable preventative healthcare benefits to young adults, such as contraception for women, pneumonia treatment, influenza vaccinations, and a number of other possibilities.
👉 Young adults in South Africa now have access to over 4,300 primary care physicians, as well as networks of hospitals and specialists, thanks to the assistance and support of this medical aid.
👉 The Bestmed Maternity Care initiative, which is available to all coverage plans, provides young expectant moms and fathers with a wealth of pregnancy and birthing information and services.
BestMed Medical Aid Plans
👉 Members can choose between BestMed Hospital Plans, Network Plans, Savings Plans, and Comprehensive Plans.
Hospital Plans
👉 Hospital Plans are popular among young adults since they cover care at a variety of network hospitals for planned and unplanned hospital stays, regardless of age. There is also the Beat1 Plan and the Beat1 Network Plan, which provide limitless coverage for unplanned hospital stays in the network’s hospitals.
Network Plans
👉 BestMed Network Plans feature a few more perks, which members who can afford somewhat higher monthly premiums appreciate:
👉 The Rhythm1 and Rhythm2 Network Plans both give unlimited in-hospital coverage with either limited critical daily benefits or comprehensive savings for consultations with certified healthcare practitioners. The Rhythm2 Network Plan is income-dependent.
Savings Plans
👉 BestMed Savings Plans are an even better option for members because they feature comprehensive hospital coverage at private hospitals as well as a savings account for normal day-to-day needs. The Network Savings plans are associated with certain Network hospitals and providers.
👉 The following options are available:
Comprehensive Plans
👉 BestMed Comprehensive Plans have the highest monthly rates and may be out of reach for many first-time subscribers. They include:
BestMed Medical Aid Waiting Period Conditions
➡️ Waiting periods can either be a general three month waiting period or a 12-month condition-specific waiting period.
➡️ Sometimes, Bestmed Medical Scheme will only pay a claim as a PMB. This happens when you are in a waiting period or when you have treatments linked to conditions that are excluded by your plan.
How Much Are BestMed Medical Aid Monthly Premiums?
👉 At the time of writing, monthly premiums for the cheapest BestMed Beat1 Network Hospital Plan started at R1 873 for a member, with an additional R1 456 for an adult dependant and R789 for a child dependant, to a maximum of 3 child dependants. Additional children join at no additional cost.
👉 The most expensive plan at the time was the Pace4 Comprehensive Plan, with monthly contributions of R10 343 per member and R10 343 per adult dependant. For a child dependant the extra contribution was R2 423, up to 3 child dependants with additional children added as beneficiaries of the scheme at no extra cost.
What Is the Waiting Period for BestMed Medical Aid’s Benefits?
👉 There can be a general waiting period of three months or a specific waiting period of 12 months for a certain condition.
👉 Bestmed Medical Scheme will sometimes only pay a claim if it is a PMB. This can happen if you are in a waiting period or if you are getting treatment for a condition that your plan doesn’t cover.
How to Claim for Benefits from BestMed Medical Aid
👉 If your healthcare provider does not submit claims to BestMed, one must submit the original claim directly to the fund administrators.
👉 You can claim by means of the BestMed App, or by scanning and emailing your claim to them.
👉 Details that should appear on all claim documents include:
➡️ Member’s name and contact details
➡️ BestMed membership number
➡️ Patient’s details
➡️ Service provider’s name, contact details and practice number
➡️ Details of treatment, including applicable tariff and ICD-10 codes
➡️ Whether payment should be done to the service provider or the member
👉 You will receive an email confirmation when your claim is received and indexed.
BestMed Medical Aid Contact Details
Head Office:
Bestmed Medical Scheme,
Glenfield Office Park
361 Oberon Avenue
Faerie Glen
Pretoria
PO Box 2297
Pretoria
Emails: [email protected]; [email protected],
Phone: +27 (0)86 000 2378
READ more about the Top Choice Holiday Travel Medical / Health Insurances in South Africa reviewed and revealed by our panel of experts.
5. Medihelp Medical Aid
Overview
👉 Medihelp is a dependable and consistent organisation that can assist members in paying for medical care.
👉 Medihelp has consistently prioritised the needs of its members since its inception more than a century ago. Medihelp remains one of the top five medical aid providers in the industry because of its ability to react to new needs and improve its business practices via the use of cutting-edge technologies.
👉 Medihelp is self-managed, with the objective of caring for its members and meeting their medical requirements.
👉 Members in South Africa can feel at ease with Medihelp, whether they are students, have recently started a new job and want to join a medical aid for the first time, are self-employed and looking for a dependable healthcare solution for their employees, or are planning a family.
👉 Medihelp, as a self-administered plan, is owned by its members, who also handle administrative activities such as processing and paying claims, obtaining pre-authorization, and communicating with members. As a result, young adults may be confident that Medihelp workers will provide them with the best assistance possible.
Medihelp Medical Aid Plans
👉 Medihelp provides a variety of options for specific plans, as follows:
MedMove
👉 Through excellent networks, Medmove delivers health necessities coverage such as private hospitalisation and emergency medical services. Members can also get virtual and in-person doctor consultations and medicine, as well as a variety of other medical services.
MedElect Student
👉 MedElect works with a high-quality network of service providers to provide comprehensive coverage at an affordable price for students. Its advantages include extensive in-hospital coverage, screenings, and additional benefits.
MedVital
👉 MedVital is an additional healthcare solution that provides low-cost coverage for small medical bills, private hospitalisation, and emergency medical services.
MedAdd
👉 MedAdd provides the flexibility of an additional savings account, additional insured cover if funds are gone, coverage for dental and eye care, and pregnancy benefits, which is a significant benefit for young families.
MedSaver
👉 MedSaver covers private hospitalisation at any hospital, while the 25% savings pocket covers out-of-hospital medical bills. When your funds are spent, an additional out-of-hospital coverage kicks in.
MedPrime, MedElite & MedPlus
👉 Due to the high monthly premiums, these top-tier plans may not be suitable for young adults.
👉 They offer private hospitalisation, exceptional out-of-hospital service coverage through a savings account, and comprehensive acute and chronic medicine, radiography, pathology, dental, and optometry benefits.
👉 Read more about MedPrime , MedElite and MedPlus
Medihelp Medical Aid Waiting Period Conditions
➡️ A general waiting period of up to three months applies from the date that you joined. During this time, you will not be entitled to any benefits except prescribed minimum benefits (PMB). If you submit claims during this waiting period, they will not be paid by the Scheme.
How Much Are Medihelp Medical Aid Monthly Premiums?
👉 Medihelp monthly premiums start with Medmove’s R1 476 per month per member for health essentials cover such as private hospitalisation and emergency medical services through networks and go up to R7,368 per month for the top-of-the-range MedElite plan that offers the most extensive cover for medical emergencies, private hospitalisation and preventive care, as well as extensive provision for acute and chronic medicine, radiology, pathology and other day-to-day medical expenses.
What Is the Waiting Period for Medihelp Medical Aid’s Benefits?
👉 Medihelp may apply a general waiting period or a condition-specific waiting period.
👉 A general waiting period of up to three months applies from the date that a member joined. During this period, a person is not entitled to any benefits except prescribed minimum benefits (PMB). Claims submitted during this waiting period, will not be paid by the scheme.
👉 During a condition-specific waiting period of up to 12 months, a member will not be entitled to benefits for a particular condition for which the person receive medical advice, a diagnosis, care or treatment (excluding PMB).
👉 Upon joining Medihelp, members receive a document with the conditions under which they are enrolled as beneficiaries, indicating any waiting periods and/or late-joiner penalties.
How to Claim for Benefits from Medihelp Medical Aid
👉 To submit a medical aid claim with Medihelp, a member can use one of the following options:
➡️ Use Medihelp’s member app to upload the account and proof of payment and submit.
➡️ Email the account and proof of payment to [email protected].
➡️ Submit your claim by logging in to Medihelp’s Member Zone and clicking on “Claims” – “Submit a claim”.
👉 To guarantee that your claim is valid according to the Medical Schemes Act and Medihelp’s Rules, ensure that you have provided the following details:
➡️ Your membership number
➡️ The member’s name and surname
➡️ The name, surname and date of birth of the patient
➡️ Medihelp Medical Scheme – not “Private” (this has tax implications)
➡️ The healthcare practitioner’s name and practice code number
➡️ The amount charged per item
➡️ The amount you have paid
➡️ Your proof of payment (attached)
➡️ The relevant codes such as ICD-10, NAPPI and item code(s)
➡️ The date on which the service/procedure was rendered/performed
👉 The account should not be modified by hand in any way, as this will cause your claim to be invalid.
👉 Your claims must reach Medihelp on or before the last workday of the fourth calendar month after the month in which the service was rendered.
Medihelp Medical Aid Contact Details
Medihelp Head Office
Postal address
PO Box 26004
Arcadia, 0007
Street address
189 Clark street,
Brooklyn, 0181
Customer care
General enquiries – 086 0100 678
International – +27 12 336 9000
Email: [email protected]
Claims submission: [email protected]
Frequently Asked Questions
What is Medical Aid in South Africa with Immediate Cover?
Immediate Cover Medical Aid in South Africa is a sort of Medical Aid that provides coverage right away, with no waiting time. This implies that you can immediately begin utilizing your benefits. Immediate Cover enables you to receive the care you require as soon as you demand it, in contrast to other types of Medical Aid that may necessitate a waiting period before you may access certain benefits.
What benefits can I expect from Medical Aid in South Africa with Immediate Cover?
Depending on the provider and the policy you select, Medical Aid in South Africa with Immediate Cover has a range of advantages. However, frequent advantages include access to specialized care, chronic medicine, and emergency medical services, as well as coverage for in- and out-of-hospital medical costs. Some insurance plans could also provide other advantages like dental and vision coverage.
Will a medical aid waive its waiting period if I am sick?
The practice of waiving waiting periods for sick people by medical aids is uncommon. Medical Aids are obligated to apply the same regulations to all individuals in similar situations, therefore if they grant you a waiting period exemption, they are also obligated to provide it to all other individuals in a similar situation.
Will medical aid in South Africa with immediate cover, cover pregnancy immediately?
Your choice of provider and particular policy will determine this. It’s crucial to thoroughly read the terms and conditions of your policy, and if you have any questions about what is covered, contact your provider directly. If you think having immediate pregnancy coverage is crucial, make sure to shop around and compare policies to locate one that works for you.
Will I be able to join a medical aid scheme with immediate cover when I have a pre-existing condition?
Even if you have a pre-existing condition, you may be able to enroll in a Medical Aid program in South Africa with instant coverage, but it will depend on the particular policy and provider you select. Pre-existing conditions may be excluded from coverage by some Medical Aid companies for a set amount of time after you sign up, while they may be covered right away by other Medical Aid companies.


































