Principle Member
From R8381
Dependant Member
From R7927
Child Dependant
From R1671
Classic Comprehensive
The Classic Comprehensive plan is designed for those who are willing to pay a premium price for top-tier medical coverage.
★★★★★ 4.5/5
Chronic Cover:
Day-to-Day:
Preventative Care:
Cancer Cover:
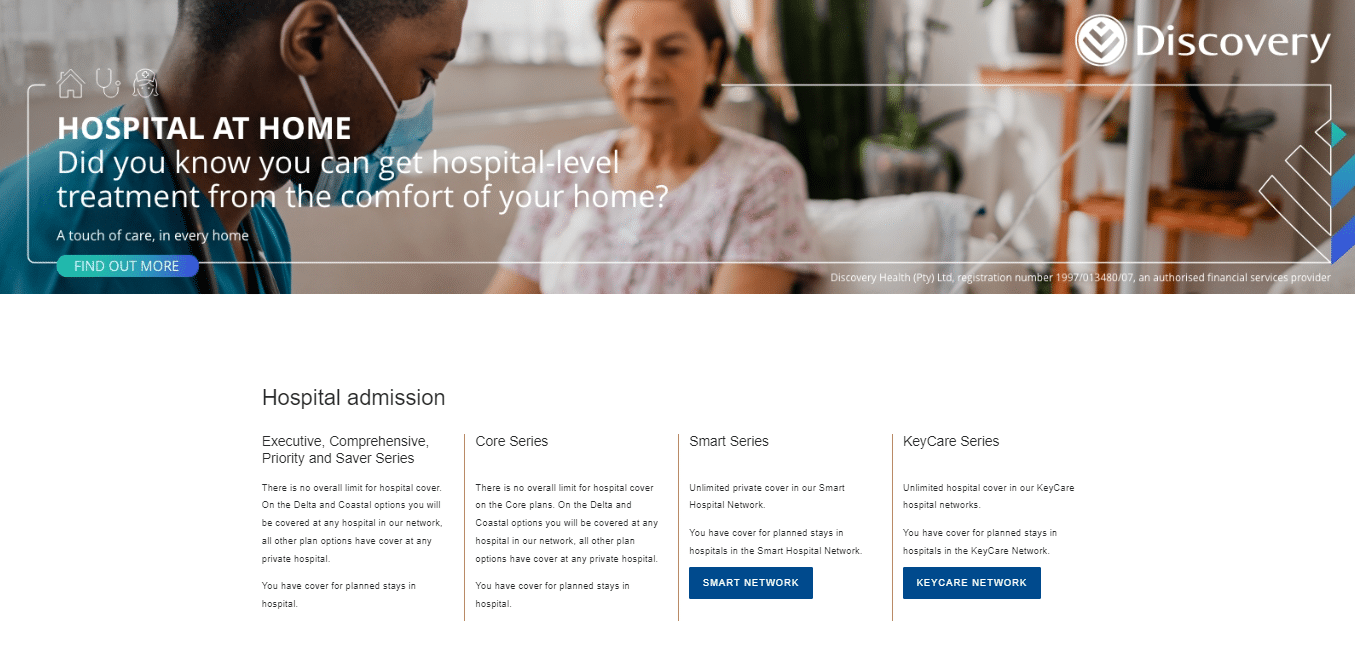
Hospitalisation:
Maternity Benefits:
The Classic Comprehensive plan is designed for those who are willing to pay a premium price for top-tier medical coverage.
Tax Deductible:
Travel Cover:

Classic Comprehensive
The Classic Comprehensive plan is designed for those who are willing to pay a premium price for top-tier medical coverage.
★★★★★ 4/5
Principle Member
From R8381
Dependant Member
From R7927
Child Dependant
From R1671
Chronic Cover:
Day-to-Day:
Preventative Care:
Cancer Cover:
Hospitalisation:
Maternity Benefits:
The Classic Comprehensive plan is designed for those who are willing to pay a premium price for top-tier medical coverage.
Tax Deductible:
Travel Cover: