- Medical Aid
- Currently Trending
The Best Medical Aids
- Compare Plans
- Gap Cover
- Best Gap Covers
- Hospital Plans
- Currently Trending
The Best Hospital Plans
- Medical Insurance
- Pet Insurance
Discovery Health KeyCare Plus Medical Aid Plan
Overall, the Discovery Health KeyCare Plus Medical Aid Plan is a trustworthy and comprehensive medical aid plan that offers 24/7 medical emergency assistance and in-hospital procedures to up to 3 Family Members. The Discovery Health KeyCare Plus Medical Aid Plan starts from R1,652 ZAR.
| 🔎 Medical Aid Plan | 🥇 KeyCare Plus |
| 👤 Main Member Contribution | R1,652 – R3,354 |
| 👥 Adult Dependent Contribution | R1,652 – R3,354 |
| 🍼 Child Dependent Contribution | R601 – R897 |
| 🔁 Gap Cover | ✅ Yes |
| 📉 Annual Limit | Unlimited Hospital Cover |
| 📈 Above Threshold Benefit (ATB) | None |
| 🌎 International Cover | None |
| 😷 Screening and Prevention | ✅ Yes |
| 💙 Medical Savings Account | None |
Discovery Health KeyCare Plus – 21 Key Point Quick Overview
- ✅ Discovery Health KeyCare Plus Overview
- ✅ Discovery Health KeyCare Plus Contributions
- ✅ Discovery Health KeyCare Plus Benefits at a Glance
- ✅ Discovery Health KeyCare Plus Benefits and Cover Comprehensive Breakdown
- ✅ Discovery Health WELLTH Fund
- ✅ Discovery Health WHO Outbreak Benefit
- ✅ Discovery Health Connected Care
- ✅ Discovery Health Hospital At Home
- ✅ Discovery Health Day-To-Day Benefits and Cover
- ✅ Discovery Maternity and Early Childhood Benefits
- ✅ Discovery Health Chronic Benefits
- ✅ Discovery Health Care Programs
- ✅ Discovery Health Comprehensive Cancer Cover
- ✅ Discovery Health Hospital Benefit
- ✅ Discovery Health KeyCare Cover for Day Surgery Network Procedures
- ✅ Discovery Health KeyCare Additional Benefits
- ✅ Discovery KeyCare Plus Value-Added Offers
- ✅ Discovery Health KeyCare Plus Exclusions and Waiting Periods
- ✅ Discovery Health KeyCare Plus Plan vs Similar Plans from Other Medical Schemes
- ✅ Our Verdict on Discovery Health KeyCare Plus
- ✅ Discovery Health KeyCare Plus Frequently Asked Questions
Discovery Health KeyCare Plus Overview
The Discovery Health KeyCare Plus starts from R1,652 and is part of a series of comprehensive medical insurance plans offered by Discovery Health.
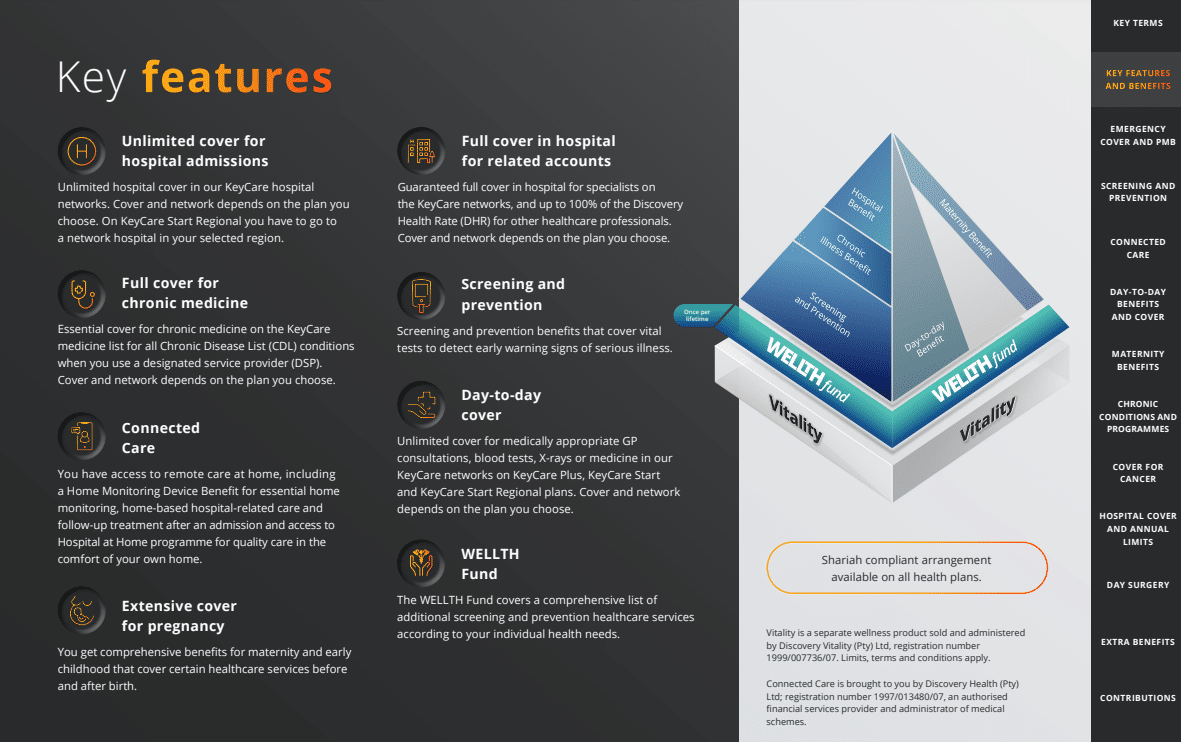
Discovery Health has the following plans to offer under the Discovery Health KeyCare series:
The KeyCare Plus plan offered by the Discovery Health Medical Scheme provides members access to affordable healthcare services through a network of hospitals and healthcare providers. Gap Cover is available on the Discovery Health Coastal Saver, along with 24/7 medical emergency assistance. According to the Trust Index, Discovery Health has a trust rating of 4.8.
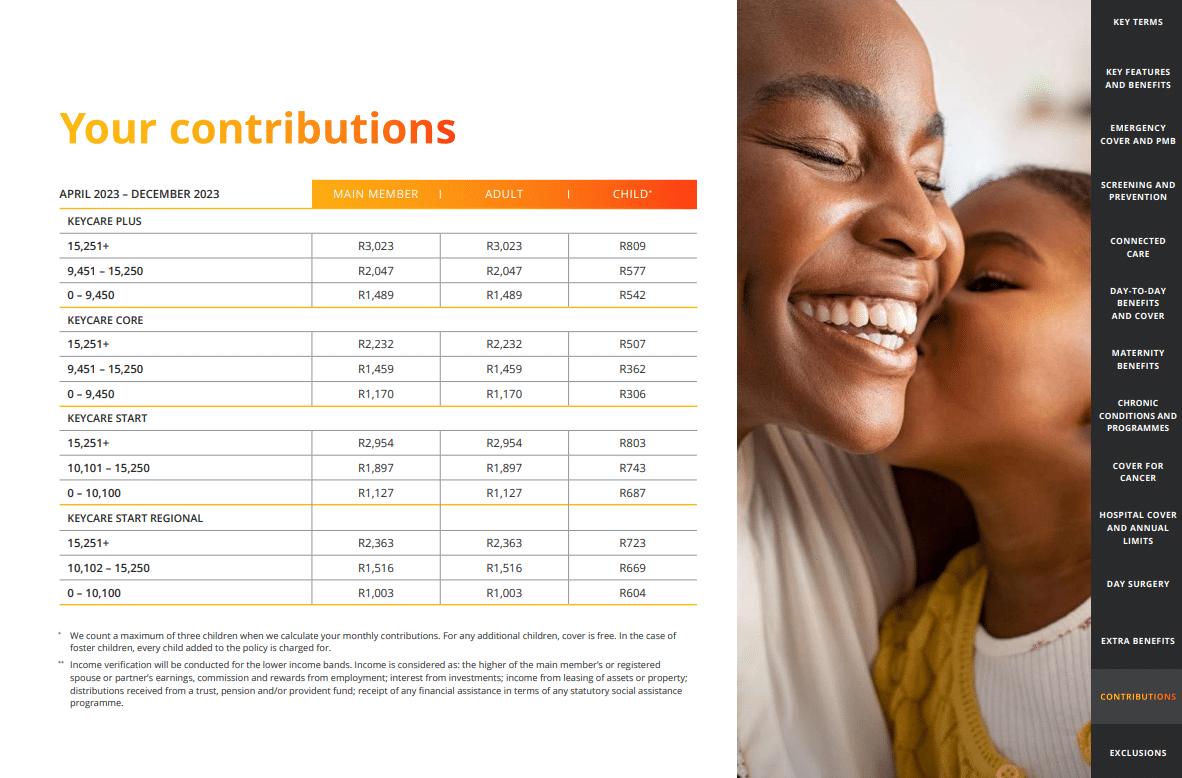
Discovery Health KeyCare Plus Contributions
| 💴 Income Level | 👤 Main Member | 👥 +1 Adult Dependent | 🍼 +1 Child Dependent |
| R15,251+ | R3,354 | R3,354 | R897 |
| R9,451 – R15,250 | R2,271 | R2,271 | R640 |
| R0 – R9,450 | R1,652 | R1,652 | R601 |
Discovery Health KeyCare Plus Benefits at a Glance
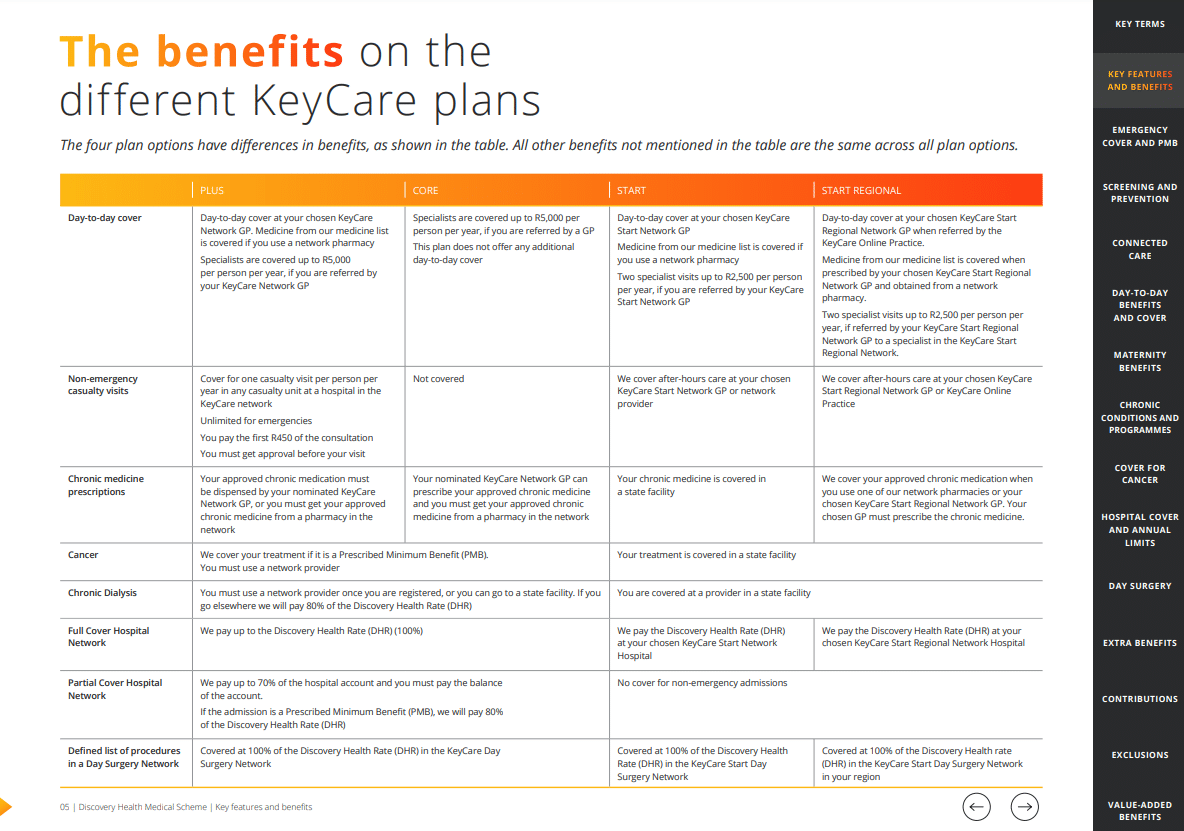
| 🟥 Day-to-Day Cover | Covers the KeyCare Network GPs. Network pharmacies cover the medicine list. If your KeyCare Network GP refers you, specialists cost up to R5,000 annually. |
| 🟧 Non-Emergency Casualty Visits | One casualty visit per year in any KeyCare hospital casualty unit. Unlimited for emergencies The consultation costs R450. Visits require approval. |
| 🟨 Chronic Medicine Prescriptions | Your KeyCare Network GP or pharmacy must dispense your approved chronic medication. |
| 🟩 Cancer | Prescribed Minimum Benefit treatment is covered (PMB). Members must use a network provider. |
| 🟦 Chronic Dialysis | Once registered, you must use a network provider or a state facility. Discovery Health will pay 80% of Discovery Health Rate if you leave (DHR) |
| 🟪 Partial Cover on the Hospital Network | Discovery Health will pay 70% of the hospital bill, and you will pay the rest. Discovery Health will pay 80% of the Discovery Health Rate for PMB admissions (DHR) |
| 🟥 Pre-defined list of approved procedures in the KeyCare Day Surgery Network | 100% Discovery Health Rate (DHR) in KeyCare Day Surgery Network. |
Discovery Health KeyCare Plus Benefits and Cover Comprehensive Breakdown
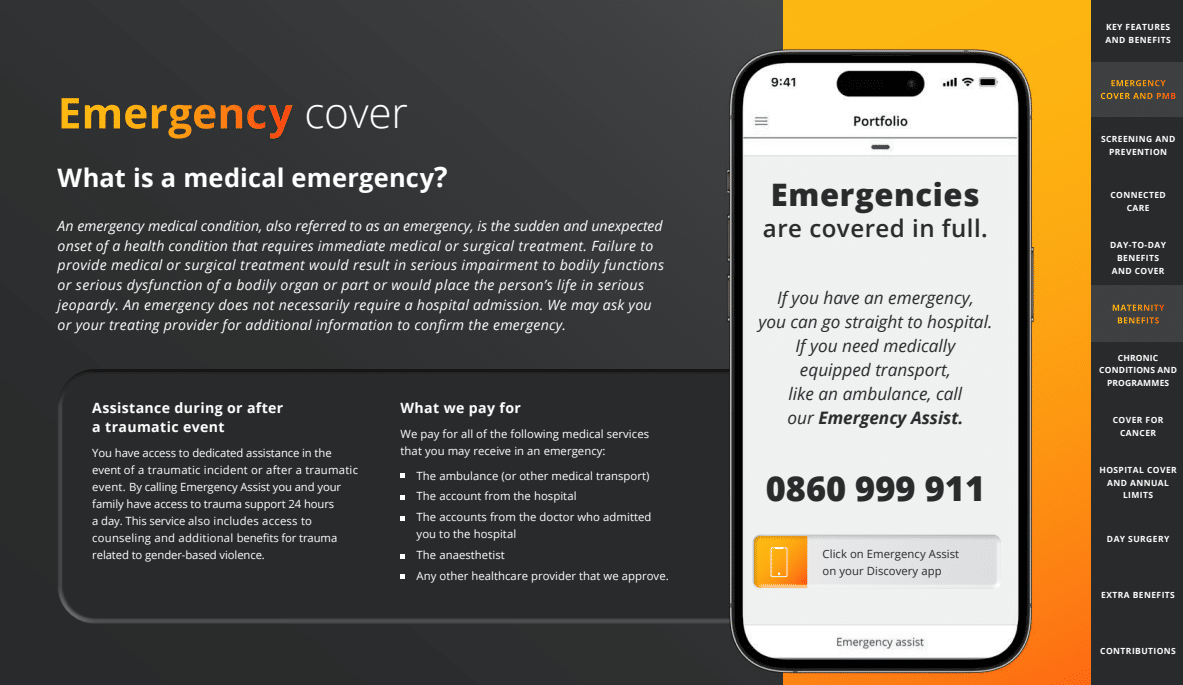
Emergency Cover
In case of a traumatic incident or after a traumatic event, you can get help from a trained professional. Calling Emergency Assist will help you and your loved ones in need. Furthermore, family members can get help after a traumatic event at any time. The survivors of gender-based violence can receive counseling and other support as part of this service.
Discovery Health Emergency Cover covers the following medical services:
- The emergency vehicle (or other medical transport).
- The hospital’s account of the incident.
- The observations of the physician who admitted you to the hospital.
- The anesthesiologist.
Any additional approved healthcare provider.
Prescribed Minimum Benefits
All medical schemes are required by the Prescribed Minimum Benefit (PMB) provisions of the Medical Schemes Act 131 of 1998 and its Regulations to cover the costs associated with the diagnosis, treatment, and care of:
- A life-threatening medical condition
- A defined listing of 271 conditions
- A list of 27 chronic illnesses.
Your medical condition must be on the Prescribed Minimum Benefit (PMB) conditions list to qualify for coverage. Furthermore, the necessary treatment must correspond to the treatments listed in the benefits. In addition, you are required to utilize designated service providers (DSPs) within the Discovery Health network. Once your condition has stabilized, you will be transferred to a hospital or other service providers in the Discovery Health network, if necessary, according to the scheme’s rules. Discovery Health will cover up to 80% of the Discovery Health Rate if you do not use a DSP (DHR). Your responsibility will be to determine the difference between what Discovery Health will pay and the actual cost of your treatment.
Furthermore, Discovery Health will pay according to your plan’s benefits if these criteria are unmet.
You might like 5 Best Medical Aids under R3000
Screening and Prevention
This benefit covers certain diagnostic procedures that detect early warning signs of serious diseases. The Discovery Health wellness providers cover a variety of screening tests, including blood glucose, cholesterol, HIV, Pap smear or HPV test for cervical screening, mammograms or ultrasounds, and prostate screenings. After all your membership members have completed their health check, you can access additional screening and preventive healthcare services through the WELLTH Fund.
The Discovery Health Screening and Prevention covers the following:
- Screening for kids will assess the child’s growth and development, including weight, height and body mass index measurements, blood pressure, and more.
- Screening for Adults includes blood pressure, blood glucose, HIV, and more. Discovery also covers mammograms, breast ultrasounds, pap smears, and more.
Screening for Seniors (65>) includes risk screening assessments and referrals to Premier Plus GPs according to the screening results.
Discovery Health WELLTH Fund
The WELLTH Fund covers a comprehensive list of screening and prevention healthcare services to empower you to act based on your individual health requirements. This benefit is distinct from and in addition to the Screening and Prevention Benefit; it is available once per lifetime to all members and dependents who have completed their health checks. Your WELLTH Fund can be used up to its maximum for screening and prevention services. However, the cover is subject to the Scheme’s clinical entry requirements, treatment protocols, and guidelines.
The Discovery Health WELLTH Fund for KeyCare Plus covers the following:
| 🅰️ General Health | You can access screenings for vision, hearing, dental, and skin conditions as part of your primary care. Additionally, you are eligible for one GP screening consultation |
| 🅱️ Physical Health | Dieticians, biokinetics, or physiotherapists are available for physical well-being evaluations. |
| ❤️ Mental Health | You have access to a mental health evaluation to promote mental health. |
| 🟥 Women and Men’s Health | You have access to various screening and prevention services for women and men. These include, for instance: Consultation with your doctor for gynecological, prostate, or cardiac issues Bone density analysis |
| 🔴 Children’s Health | A pediatrician, speech pathologist, or physiotherapist can evaluate your child’s progress toward important developmental milestones as part of a well-child check-up. |
| 🚩 Medical Monitoring Devices | You have access to medical monitoring devices that assist in measuring, for instance, blood pressure, cholesterol, and blood sugar. |
The WELLTH Fund is available for two benefit years after all beneficiaries over two complete an age-appropriate health check with a Wellness Network provider. Furthermore, the benefit is available to new members in the joining year and subsequent years. The benefit is available once per lifetime per beneficiary. Cover for eligible healthcare services is limited to the Discovery Health Rate (DHR), subject to the overall benefit maximum.
Your WELLTH Fund maximum is based on the size and composition of your family as stated in your policy:
- Limited to R2,500 per adult dependent.
- Limited to R1,250 per two-year-old or older child dependent.
- Limited to R10,000 per family.
Furthermore, the WELLTH Fund is available to all registered membership beneficiaries and will not cover healthcare services already covered by other defined benefits.
Discovery Health WHO Outbreak Benefit
The basket of care includes the following:
- ✅ COVID-19 vaccines and their administration according to the COVID-19 guidelines of the National Department of Health.
- ✅ Screening consultations with a network general practitioner (virtual, telephone, or in-person).
- ✅ COVID-19 PCR and Rapid Antigen screening tests if referred by a qualified medical practitioner.
- ✅ A set of defined pathology tests for COVID-19-positive individuals.
- ✅ A predetermined assortment of x-rays and scans for COVID-19-positive individuals.
- ✅ Members at risk who meet the clinical entry criteria will receive supportive care, including medication and a home monitoring device to track oxygen saturation levels.
- ✅ When you are admitted to the hospital because of symptoms of COVID-19, you will be covered by the Hospital Benefit of the KeyCare Plus and, if necessary, the PMBs.
- ✅ Access to the Long COVID Recovery Program.
How members of the Discovery Health KeyCare Plus are covered in terms of Monkeypox:
- ✅ The treatment protocol for confirmed cases consists of a diagnostic PCR screening test
- ✅ Two visits to a dermatologist or general practitioner.
Formulary of supportive medications for pain management.
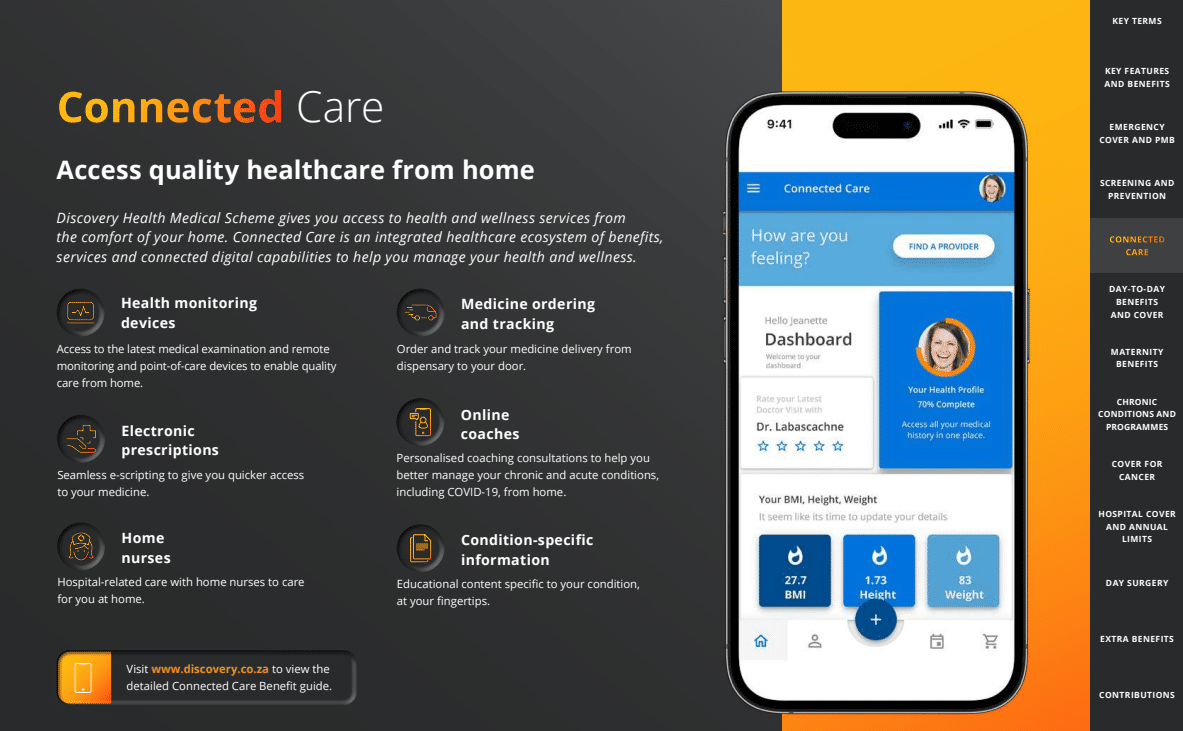
Discovery Health Connected Care
Discovery Health Medical Scheme provides home-based access to health and wellness services. Connected Care is an integrated ecosystem of benefits, services, and digitally connected capabilities designed to assist you in managing your health and wellness.
| 🟥 Health Monitoring Devices | Access to the most up-to-date medical examination, remote monitoring, and point-of-care devices to facilitate the delivery of quality care at home. |
| 🟧 Electronic Prescriptions | Electronic prescribing for expedited access to medications. |
| 🟨 Home Nurses | Hospital-related care is provided at home by registered nurses. |
| 🟩 Medicine Ordering and Tracking | Order and track the delivery of your medication from the dispensary to your door. |
| 🟦 Online Coaches | At-home consultations with a coach to help you better manage your chronic and acute conditions, including COVID-19. |
| 🟪 Condition-Specific Information | Educational content pertinent to your condition is readily accessible. |
✅ Connected care for members at home
Previously unimaginable access to medical professionals is now at your fingertips, thanks to the advent of online consultations. Thanks to the Home Monitoring Device Benefit, you can get various approved home monitoring devices for chronic and acute conditions. You will not see any changes to your regular benefits because of having cover approved for these gadgets.
✅ Connected care for those with chronic conditions
Through Connected Care, you and your doctor can work together to keep your chronic condition under control while you are at home.
You might also like 5 Best Medical Aids for Chronic Illness Cover
Eligible members can use various digital services connected to smart remote monitoring, point-of-care devices, and individualized coaching consultations to monitor and control their chronic condition in the comfort of their homes.
Discovery Health Hospital At Home
Hospital at Home patients receive specialized care from a dedicated medical staff in the comfort of their own homes. Each of these benefits and services contributes to your overall health and well-being. They all work together to make your healthcare more efficient and your life safer. Suppose you have a valid pre-authorization for hospitalization. In that case, Discovery Health will use your Hospital Benefit to cover any services provided as part of Discovery’s Hospital at Home program. For those who meet the program’s clinical and benefit criteria, this unlocks cover for approved medical devices and services.
✅ Furthermore, Discovery Health covers the following:
- 24/7 clinical oversight from a care team virtually, including nurses, doctors, and allied healthcare professionals.
- 24/7 real-time remote monitoring, which is supported by innovative healthcare technology.
- Hospital-level diagnostics and intervention to manage post-surgical or medical care at home.
POLL: 3 Best Hospital Plans Under R1000
✅ Acute Care at home
This includes cover and treatment for COVID-19, as well as post-discharge care. In addition, you are eligible for the Home Monitoring Device Benefit.
✅ Home Monitoring Devices
- Suppose you meet the Scheme’s clinical entry criteria. In that case, you have healthcare coverage up to a limit of R4,250 per person per year at 100% of the Discovery Health Rate (DHR) for monitoring certain conditions like chronic obstructive pulmonary disease, congestive heart failure, diabetes, pneumonia, and COVID-19.
- If you meet the clinical entry criteria, the scheme covers up to 75% of the Discovery Health Rate (DHR) for defined point-of-care medical devices. You are responsible for 25% of the total cost of these devices. In addition, you have access to the most advanced remote medical examination device, known as TytoHome.
- TytoHome enables you to conduct a medical examination by transmitting throat, ear images, and heart and lung sound to your doctor in real time.
✅ Home Care Cover
- Discovery Home Care is a service that provides you with high-quality care in the comfort of your own home if your doctor recommends it as an alternative to hospitalization. Postnatal care, end-of-life care, intravenous infusions (drips), and wound care are provided. These services are covered by the Hospital Benefit, pending authorization.
- Discovery Home Care is the designated service provider (DSP) for intravenous infusion administration. Use Discovery Home Care for these infusions to avoid a 20% co-payment.
✅ Home-based care for follow-up treatment after hospital admission
- Once discharged from the hospital, patients with clinically appropriate conditions such as chronic obstructive pulmonary disease, chronic cardiac failure, ischemic heart disease, and pneumonia have access to enhanced home-based care.
- If you meet the clinical entry criteria, you are covered for bedside medicine reconciliation before admission discharge, a follow-up consultation with a GP or specialist, and a defined basket of supportive care at home, including in-person and virtual consultations with a Discovery Home Care nurse.
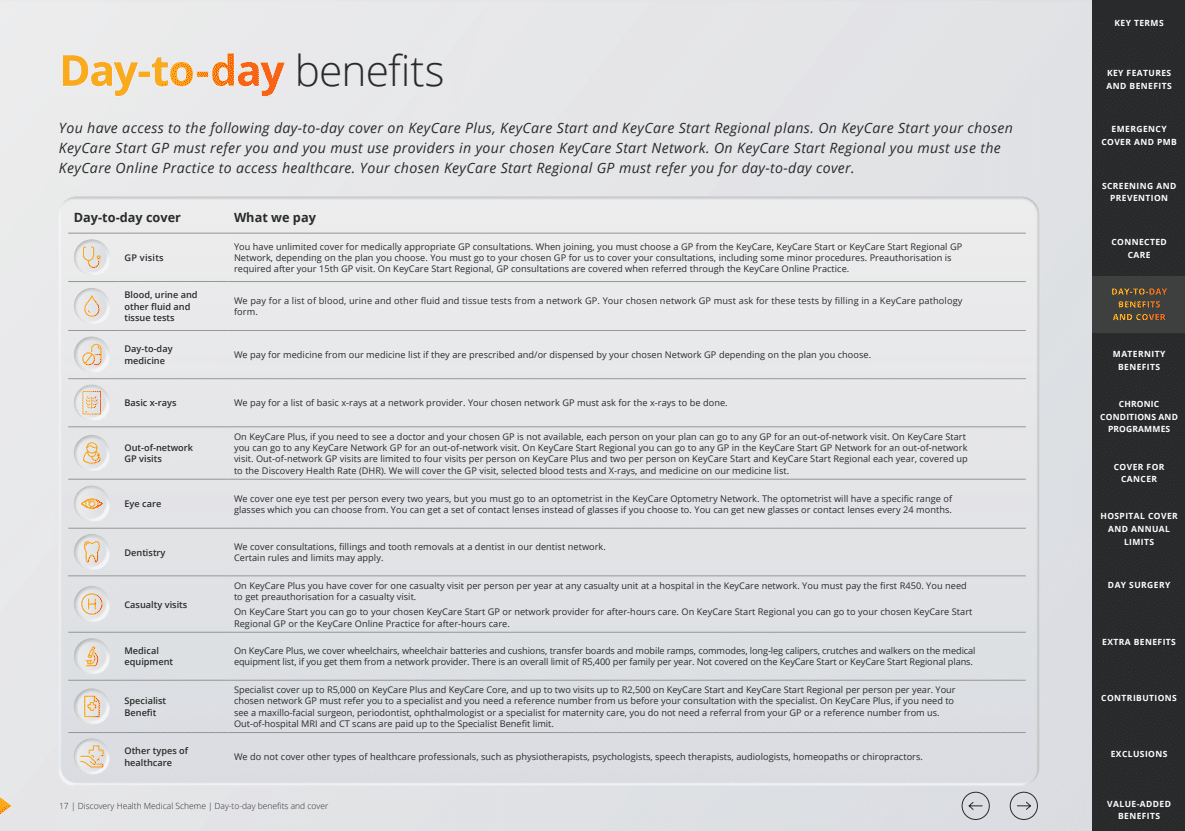
Discovery Health Day-To-Day Benefits and Cover
| 🩺 General Practitioner (GP) Visits | Medically necessary GP consultations are unlimited. You must choose a KeyCare Regional GP when joining. Discovery Health will cover consultations and minor procedures at your chosen GP. Pre-authorization is needed after 15 GP visits. |
| 🩸 Blood, urine, and other fluid and tissue tests | Discovery Health will cover network GP blood, urine, and other fluid and tissue tests. These tests require a KeyCare pathology form from your network GP. |
| 🧬 Day-to-day Medicine | Depending on your plan, Discovery Health will cover the medicine list if your Network GP prescribes and dispenses it. |
| 🩹 Basic X-Rays | Discovery Health will pay for network-provided basic X-rays. However, your network GP must order X-rays. |
| 🅰️ Out-of-Network GP Visits | KeyCare Plus allows you to see any GP out-of-network if your preferred GP is unavailable. The Discovery Health Rate covers up to four out-of-network GP visits per year on KeyCare Plus. The Discovery Health medicine list, GP visits, selected blood tests, and X-rays are covered. |
| 🅱️ Eyecare | You can get one eye exam every two years at a KeyCare Optometry Network optometrist. The optometrist will offer specific glasses. Contact lenses can replace glasses. Glasses and contacts can be replaced every 24 months. |
| 🦷 Dentistry | Our dentist network covers consultations, fillings, and tooth extractions. Limits may apply. |
| 📌 Casualty Visits | KeyCare Plus covers one casualty visit annually at any KeyCare hospital casualty unit. There is a co-payment of R450. Casualty visits require pre-authorization. |
| 📍 Medical Equipment | If you get medical equipment from a network provider, KeyCare Plus covers wheelchairs, batteries, cushions, transfer boards, mobile ramps, commodes, long-leg calipers, crutches, and walkers on the medical equipment list. The annual family limit is R5,400. |
| ➡️ Specialist Benefit | Limited to two visits to a specialist up to R5,000 annually. Before seeing a specialist, your network GP must refer you and provide a reference number. You do not need a GP referral or reference number to see a maxillo-facial surgeon, periodontist, ophthalmologist, or maternity care specialist on KeyCare Plus. The Specialist Benefit covers out-of-hospital MRI and CT scans. |
| ↪️ Alternative Healthcare | Physiotherapists, psychologists, speech therapists, audiologists, homeopaths, and chiropractors are excluded from cover on all KeyCare plans. |
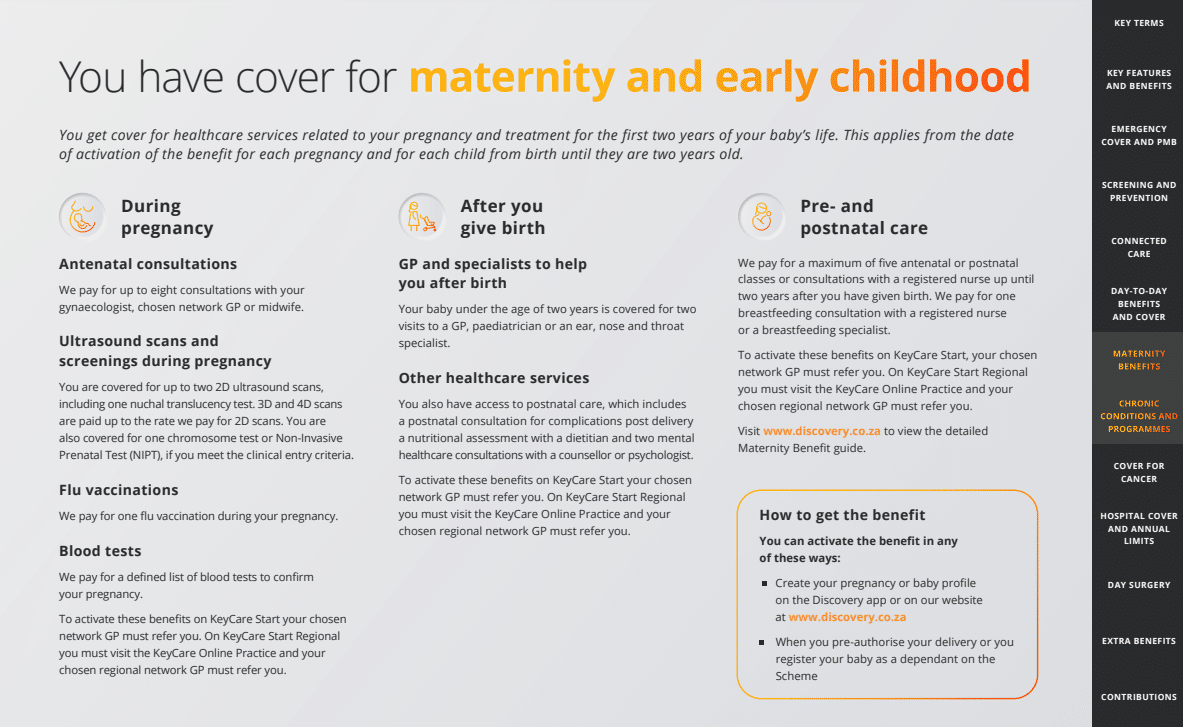
Discovery Maternity and Early Childhood Benefit
With Discovery Health KeyCare Plus, you get coverage for healthcare services related to your pregnancy and treatment for the first two years of your baby’s life. This applies from the date of activation of the benefit for each pregnancy and each child from birth until they are two years old. Discovery Health Maternity Benefit covers the following:
✅ During Pregnancy:
- Scans and Screenings
- Eight antenatal consultations with a midwife, GP, or gynecologist.
- 2 x 2D ultrasound scans
- Nuchal translucency test
- 3D and 4D scans up to the 2D scan rate.
- Non-invasive Prenatal Test (NIPT)
- One flu vaccination during pregnancy.
- Discovery Health will cover predetermined blood tests to confirm your pregnancy.
READ more: 5 Best Medical Aids for Babies in South Africa
✅ After giving birth, Discovery Health covers the following:
- GP and Specialist help for up to 2 years.
- Postnatal care, including complications during delivery, nutritional assessment, etc.
Discovery Health’s prenatal and postnatal care includes Five antenatal or postnatal classes and One Breastfeeding consultation.
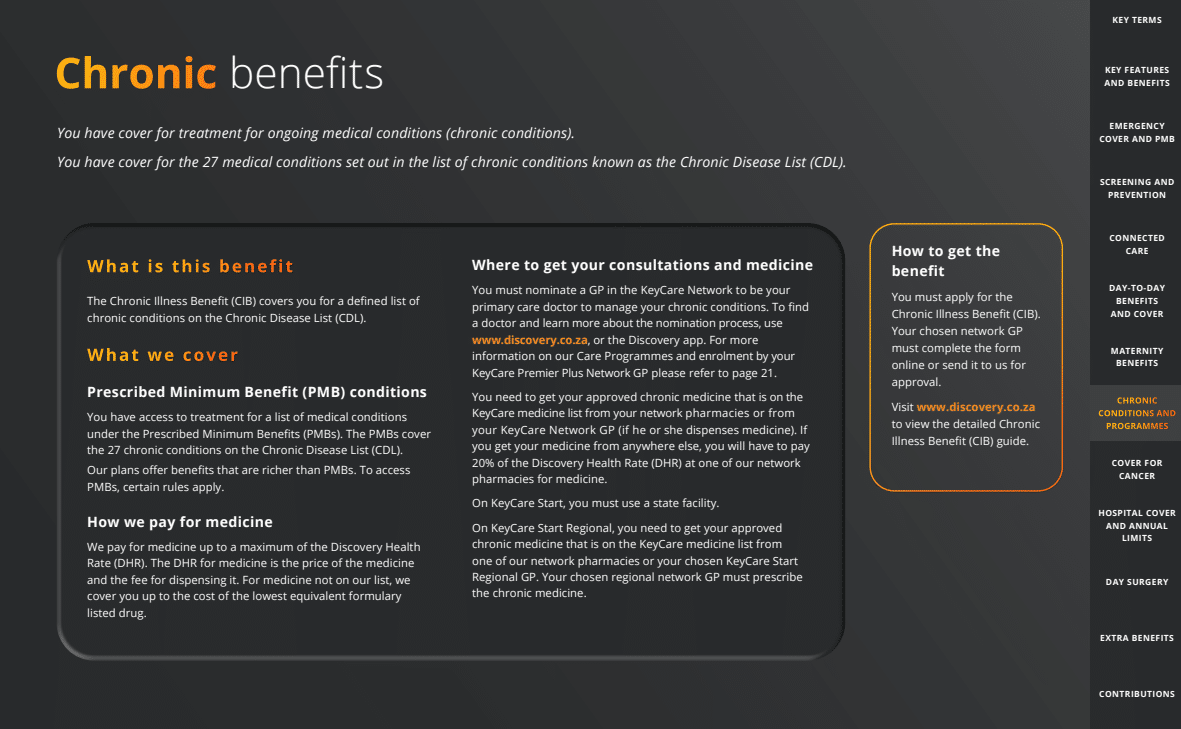
Discovery Health Chronic Benefits
The Chronic Disease List lists 27 conditions for which the Chronic Illness Benefit (CIB) provides cover (CDL).
✅ Discovery Health Chronic Benefit Cover Summarized
| 🅰️ Prescribed Minimum Benefit (PMB) Conditions | Under the Prescribed Minimum Benefits, you can receive treatment for a set of medical conditions (PMBs). The PMBs cover the 27 chronic conditions in the Chronic Disease List (CDL). |
| 🅱️ Medicine Cover for the Chronic Disease List | Discovery Health will pay for medications up to the Discovery Health Rate maximum (DHR). The DHR for medication consists of the price of the medication and the dispensing fee. The scheme will cover up to the cost of the cheapest equivalent drug on the formulary for medications not on the list. |
Discovery Health KeyCare Plus Full List of conditions covered:
- Addison’s disease
- Asthma
- Bipolar mood disorder
- Bronchiectasis
- Cardiac failure
- Cardiomyopathy
- Chronic obstructive pulmonary disease
- Chronic renal disease
- Coronary artery disease
- Crohn’s disease
- Diabetes insipidus
and many more.
Chronic Medicine
On KeyCare Plus, you can get your medication from over 2,500 pharmacies in the Scheme’s pharmacy network. Through MedXpress, you can order or reorder your medication online and have it delivered to your place of business or residence. Alternatively, you can:
- You can order your medication online and pick it up at a MedXpress Network Pharmacy or
- Fill a prescription as usual at any pharmacy in the MedXpress Network.
✅ Additional Chronic Benefits on the KeyCare Plus
Chronic Dialysis
If Discovery Health has approved your treatment plan and you use a provider in the network, Discovery Health will cover all costs associated with your chronic dialysis. Furthermore, Discovery Health will pay up to 80% of the Discovery Health Rate if you go elsewhere (DHR).
✅ Member Care Program
- If you have been diagnosed with one or more chronic diseases, you may be eligible for the Discovery Health Member Care Program.
- Discovery Health will confirm your eligibility by contacting you.
- The program provides coordinated care to help you manage your conditions and obtain the highest standard of healthcare.
- If you are registered and participate in the program, Discovery Health will fully cover your treatment’s cost.
- If you choose not to participate, Discovery Health will pay up to 80% of the Discovery Health Rate for your hospital and related bills (DHR)
✅ Medicine Tracker
You can set reminders and prompts to help you take your medication as prescribed and on time. For example, your approved chronic medication will be displayed automatically, and you will be prompted to take your medication and confirm each dose.
Discovery Health Care Programs
Discovery Health will cover preventative and condition-specific care programs that assist with managing diabetes, mental health, HIV, and heart-related conditions. You must be registered with these condition-specific care programs to access additional benefits and services. On a personalized dashboard, you and your Premier Plus GP can identify the next steps to manage your condition and optimally maintain your health over time.
| 1️⃣ Discovery Health Disease Prevention Program | KeyCare Plus GPs can enroll you in the Disease Prevention Program if you have cardiometabolic risk syndrome. GPs, dietitians, and health coaches coordinate care. In addition, consultations, pathology tests, and medicine are covered for enrolled members. Health coaching will help you manage your condition daily. |
| 2️⃣ Discovery Health Mental Health Care Program | GPs can enroll cardiometabolic risk syndrome patients in the Disease Prevention Program. Dietitians, health coaches, and GPs coordinate care. Enrolled members receive medicine, pathology, and consultations. Health coaching assists with daily management. |
| 3️⃣ Discovery Health Diabetes Care Program | Your KeyCare Plus GP can enroll you in the Diabetes Care Program if you receive the Chronic Illness Benefit (CIB) for diabetes. The program covers extra glucometer strips and dietitian and biokinetics visits. A nurse educator can help you manage your condition. |
| 4️⃣ Discovery Health HIV Care Program | KeyCare Plus GPs register HIV patients for care, including social worker cover. Guaranteed confidentiality. Avoid a 20% co-payment by getting your medicine from a DSP. |
| 5️⃣ Discovery Health Cardio Care Program | If referred by your KeyCare Plus GP and enrolled in the Cardio Care Program, you can receive a defined basket of care and an annual cardiovascular assessment if you are on the Chronic Illness Benefit (CIB) for hypertension, hyperlipidemia, or ischemic heart disease. |
The cover is subject to the Scheme’s clinical entry requirements, treatment protocols, and guidelines.
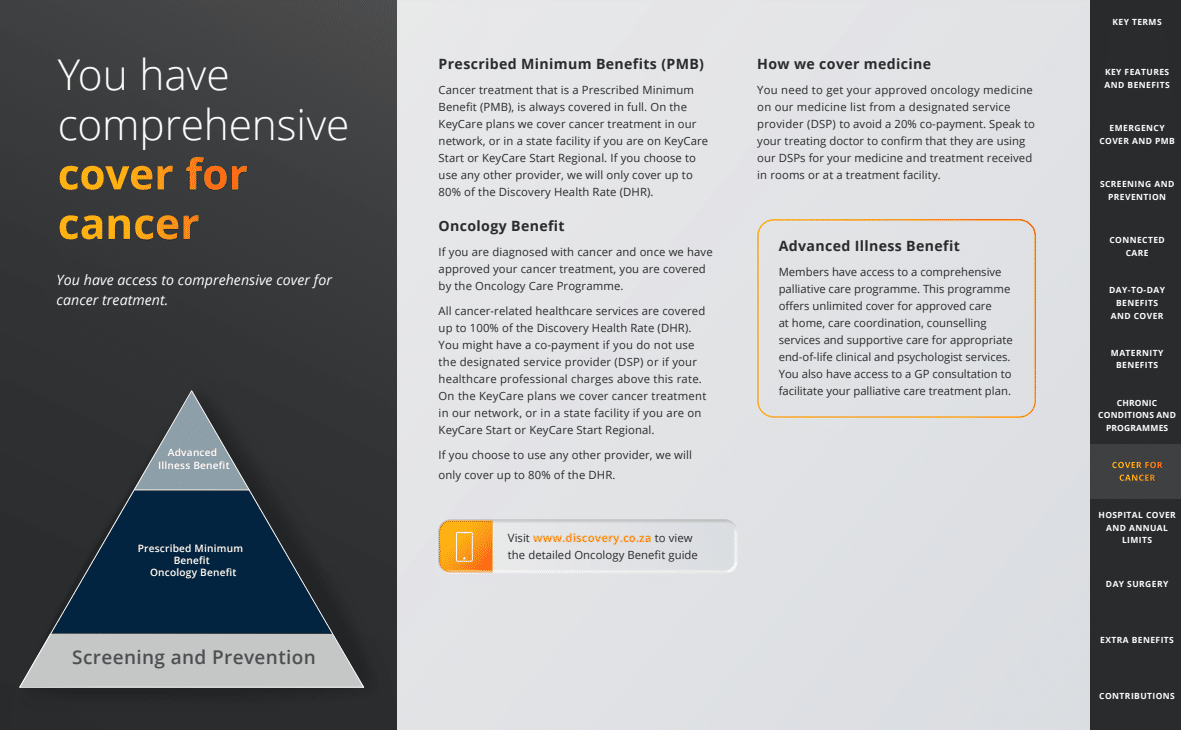
Discovery Health Comprehensive Cancer Cover
You have access to comprehensive cancer treatment coverage. This includes access to expensive medications, innovative treatments, and extended cancer coverage once certain thresholds are reached.
| ➡️ Discovery Health Prescribed Minimum Benefits (PMB) | PMB cancer treatment is always covered. |
| 🎗️ Discovery Health Oncology Benefit | After Discovery Health approves your cancer treatment, the Oncology Care Program covers you. Discovery Health Rate covers 100% of cancer-related healthcare services (DHR). If you do not use the DSP or your doctor charges more, you might have to pay a co-payment. |
| 💊 Discovery Health – Covering Medicine | To avoid a 20% co-payment, get your approved oncology medicine from a DSP on the Scheme’s medicine list. Ask your doctor if they use the Scheme’s DSPs for your in-room or facility treatment. |
| ↪️ Discovery Health Advanced Illness Benefit | Members receive comprehensive palliative care. This program covers unlimited home care, care coordination, counseling, and supportive care for appropriate end-of-life clinical and psychologist services. Your palliative care treatment plan includes GP consultations. |
Discovery Health Hospital Benefit
KeyCare Plus includes hospitalization coverage. Furthermore, there is no limit on the total amount covered by Hospital Benefits.
- If you require hospitalization, Discovery Health will cover your hospital bills.
- There is no annual overall hospital limit on any of the plans. However, there are maximum reimbursement amounts for certain treatments.
- Discovery Health may not cover the expenses if you do not contact the scheme before being discharged.
The following table summarizes how Discovery Health pays for approved hospital admissions with KeyCare Plus.
| 🏥 Full Cover Hospital Network | Discovery will pay a 100% Discovery Health Rate (DHR). You can use any KeyCare Network-approved hospital. |
| ⚠️ Partial Cover Hospital Network | Discovery Health will pay up to 70% of the hospital bill, and you will pay the rest. Discovery Health pays up to 80% of Discovery Health Rate for Prescribed Minimum Benefit admissions (DHR). |
| 📌 list of procedures that can be performed in a Day Surgery Network | KeyCare Day Surgery Network-covered. |
| 📍 Defined List of procedures that can be performed in specialist rooms | The Scheme-approved rate. |
| Cover for non-network hospitals | Discovery Health will not cover you if you are admitted to a non-network hospital for a planned procedure. Discovery Health pays 80% of the Discovery Health Rate for PMB admissions (DHR). |
| ➡️ Cover for Specialists and Healthcare Providers in the Discovery Health network | Full cover provided. |
| ↪️ Cover for Specialists and Healthcare Providers, not in the Discovery Health network | Paid according to the Discovery Health Rate (DHR). The member must pay the balance if they charge more. |
| 📉 Radiology and Pathology Accounts | According to the Discovery Health Rate (DHR). |
| 📈 Cover for scopes | KeyCare Day Surgery Network PMB. Hospital Benefit covers doctor-ordered scopes. |
| 🍹 Alcohol and Drug Rehabilitation | Discovery Health covers 21 days of rehabilitation per person per year. Three days for detoxification per approved admission. |
| 🧠 Mental Health Cover | Mental well-being 21 days for admissions or up to 15 outpatient consultations per person for major affective disorders, anorexia, and bulimia; up to 12 outpatient consultations for acute stress disorder accompanied by recent significant trauma. Three days per approved admission for attempted suicide. Twenty-one days for other mental health admissions. All mental health admissions are fully covered at network facilities. If you go elsewhere, Discovery Health will pay up to 80% of the Discovery Health Rate (DHR) for your hospital bill. |
READ more 10 Best Hospital Plans in South Africa
Discovery Health KeyCare Cover for Day Surgery Network Procedures
Discovery Health will cover planned day surgery procedures. The network for a day surgery depends on the plan you choose. Furthermore, these services are covered by your Hospital Benefit. As a result, Discover Health will pay for hospitalization-related services, including all authorized healthcare professionals, services, and medications. Utilize physicians, specialists, and other healthcare professionals with whom Discovery Health has a payment arrangement. The scheme will cover the full cost of these services.
The following list provides the procedures that can be performed in a Discovery Health Day Surgery Network:
- ✅ Biopsies
- ✅ Breast Procedures
- ✅ Ear, nose, and throat procedures
- ✅ Eye Procedures
- ✅ Ganglionectomy
- ✅ Gastrointestinal scopes and procedures
and many more.
Discovery Health KeyCare Additional Benefits
✅ International Second Opinion Services
- The Clinic by Cleveland Clinic provides second opinions for life-threatening and life-changing conditions through your specialist.
- Discovery Health will pay 75% for second opinions.
✅ Claims Relating to Traumatic Events
- Trauma Recovery Extender Benefit covers out-of-hospital trauma claims.
- The Trauma Recovery Extender Benefit pays claims for the rest of the year and the year after.
- During the year that the trauma occurs and the year after, you and your dependents on your health plan can receive six counseling sessions per person per year from a psychologist, clinical social worker, or registered counselor.
- To qualify, members must apply for this benefit.
✅ In-Room Procedures
- The cover is limited to a defined list of specialist room procedures.
- The cover is paid according to the agreed rate, where Discovery Health has authorized it, and the Hospital Benefit pays it.
✅ Advanced Illness Benefit
- Members receive comprehensive palliative care.
- This program covers unlimited home care, care coordination, counseling, and supportive care for appropriate end-of-life clinical and psychologist services.
Your palliative care treatment plan includes GP consultations.
Discovery KeyCare Plus Value-Added Offers
- ✅ Healthy Care at Clicks or Dis-Chem offers discounts on personal and family products. Healthy Care includes baby care, dental care, eye care, foot care, sun care, hand care, first aid, and over-the-counter medicine.
- ✅ Your plan’s optometrists offer 20% off frames and lenses when you pay immediately.
- ✅ Expectant parents can cryogenically store their newborn baby’s umbilical cord blood and tissue stem cells at a discounted rate with Netcells’ exclusive offer.
- ✅ Vitality, the world’s leading science-based wellness program, rewards healthy living. As a result, Discovery Vitality members live longer and healthier lives.
Discovery Health collaborates with myHealthTeam, a global leader in online patient communities. This gives members with diabetes, heart disease, and long-term COVID access to a digital community of patients to manage their conditions.
Discovery Health KeyCare Plus Exclusions and Waiting Periods
✅ Exclusions include the following:
- Reconstructive surgical procedures and treatments, including cosmetic procedures and treatments.
- Otoplasty for bat ears, blepharoplasty, and port-wine stains (eyelid surgery).
- Breast reductions or augmentations and gynecomastia are considered cosmetic procedures.
- Obesity
- Unless included in Prescribed Minimum Benefits (PMBs) or Assisted Reproductive Therapy, infertility is not covered (ART) Benefit.
- Frail care
- Abuse of alcohol, drugs, or solvents.
- Willful and significant infraction of the law.
- Willful participation in a war, a terrorist act, a riot, a civil disturbance, a revolt, or an uprising.
- Injuries incurred or medical care rendered during travel to or within a country at war.
- Experimental, unproven, or unregistered treatments or practices.
- Rescue and search.
✅ Additional exclusions that only apply to the KeyCare Plus include hospitalizations caused by the following, among other things:
- Dentistry
- Nail disorders
- Skin conditions, such as benign growths and lipomas
- Investigations
- Functional nasal surgery
- Elective cesarean section, unless medically required
- Hiatus hernia and esophageal reflux surgery.
- Back and neck surgery or treatment
- Knee and shoulder operations
- Arthroscopy
- Hips, knees, shoulders, and elbows are among the joints that can be replaced.
- Cochlear implants, auditory brain implants, and internal nerve stimulators (including related procedures, devices, processors, and hearing aids) are included in this category.
and many more.
✅ Discovery Health’s waiting periods are as follows:
- During your waiting periods, you will not have access to the Prescribed Minimum Benefits (PMBs) if you are subject to waiting periods due to never having belonged to a medical scheme or a break in membership of more than 90 days before joining Discovery Health Medical Scheme, including emergency admission cover.
If you had less than a 90-day break in cover before enrolling in Discovery Health Medical Scheme, you might be eligible for Prescribed Minimum Benefits (PMBs) during waiting periods.
Medical Aid Comparisons : Discovery Health KeyCare Plus Plan vs Similar Low Cost Medical Aid Plans
| 🔎 Medical Aid Plan | 🥇 KeyCare Plus | 🥈 Platinum Health PlatCap | 🥉 Bonitas BonStart |
| 👤 Main Member Contribution | R1,652 – R3,354 | R1,213 – R2,771 | R1,338 |
| 👥 Adult Dependent Contribution | R1,652 – R3,354 | R1,213 – R2,771 | R1,338 |
| 🍼 Child Dependent Contribution | R601 – R897 | R495 – R963 | R1,338 |
| 🔁 Gap Cover | ✅ Yes | None | ✅ Yes |
| 📉 Annual Limit | Unlimited Hospital Cover | Unlimited Hospital and other benefits | Unlimited Hospital Cover |
| 📈 Above Threshold Benefit (ATB) | None | None | None |
| 🌎 International Cover | None | None | R10 million |
| 😷 Screening and Prevention | ✅ Yes | None | ✅ Yes |
| 💙 Medical Savings Account | None | None | None |
You might consider reading more about Health Insurance
Our Verdict on Discovery Health KeyCare Plus
KeyCare Plus is a medical aid plan offered by the Discovery Health Medical Scheme in South Africa. It is designed to provide affordable healthcare to members through a network of hospitals and healthcare providers. One of the main features of KeyCare Plus is its unlimited coverage in the KeyCare Hospital Network, which includes private hospitals and day clinics across South Africa. As a result, members have access to various healthcare services, including specialist consultations, radiology, pathology, and hospitalization. In addition to hospital cover, KeyCare Plus also includes benefits for optometry and dental services. Members can enjoy a range of preventative and basic dental treatments, including annual check-ups, cleaning, and fillings.
The optometry benefit covers eye tests, frames, lenses, and certain contact lenses. These benefits can help members maintain good eye and dental health and prevent more serious health issues from developing. However, members should be aware of some drawbacks to the KeyCare Plus plan. Firstly, maternity coverage is limited and only covers the cost of childbirth in a KeyCare Hospital. There is no cover for postnatal care or any complications that may arise during pregnancy or childbirth.
Secondly, the plan does not include a medical savings account, meaning members must pay for certain out-of-hospital expenses out of their own pockets. Finally, the plan does not cover the cost of internal or external prostheses, such as hearing aids or artificial limbs.
You might be interested in other Discovery Health KeyCare Options:
🚩 Discovery Health Keycare Core
🚩 Discovery Health KeyCare Start
🚩 Discovery Health KeyCare Start Regional
Discovery Health KeyCare Plus Frequently Asked Questions
What is the KeyCare Hospital Network?
The KeyCare Hospital Network is a network of private hospitals and day clinics across South Africa that provide unlimited coverage for KeyCare Plus members. This means that members can receive hospitalization and related medical services at any of these facilities without worrying about exceeding their benefit limits.
What optometry benefits are included in KeyCare Plus?
KeyCare Plus includes benefits for basic optometry services such as eye tests, frames, lenses, and certain contact lenses. Members can visit any provider in the KeyCare Network for these services.
What dental benefits are included in KeyCare Plus?
KeyCare Plus includes benefits for preventative and basic dental treatments, including annual check-ups, cleaning, and fillings. Members can visit any provider in the KeyCare Network for these services.
What is the maternity cover in KeyCare Plus?
KeyCare Plus provides limited maternity cover that covers the cost of childbirth in a KeyCare Hospital. However, there is no cover for postnatal care or any complications that may arise during pregnancy or childbirth.
Does KeyCare Plus include a medical savings account?
No, KeyCare Plus does not include a medical savings account. Unfortunately, this means that members must pay for certain out-of-hospital expenses out of their own pockets.
Does KeyCare Plus cover the cost of prostheses?
No, KeyCare Plus does not cover the cost of internal or external prostheses such as hearing aids or artificial limbs. Members must pay for these items out of their own pockets or through other benefits or plans.
You might also like
Table of Contents
Free Medical Aid Quote
Our Trusted Partners
We work with leading medical aid companies in South Africa.

7 Actionable Ways to save 32% on your MEDICAL AID in 14 days.

- +27 72 7967 530
- [email protected]
- 2nd Floor, West Tower, Nelson Mandela Square, Sandton, 2196, Johannesburg, Gauteng, South Africa
🔎 Report a bug or outdated data to be updated to [email protected]
© Medicalaid.com | All rights Reserved |
Copyright 2024
Top 5 Medical Aids
Top 5 Gap Cover Plans
































