- Medical Aid
- Currently Trending
The Best Medical Aids
- Compare Plans
- Gap Cover
- Best Gap Covers
- Hospital Plans
- Currently Trending
The Best Hospital Plans
- Medical Insurance
- Pet Insurance
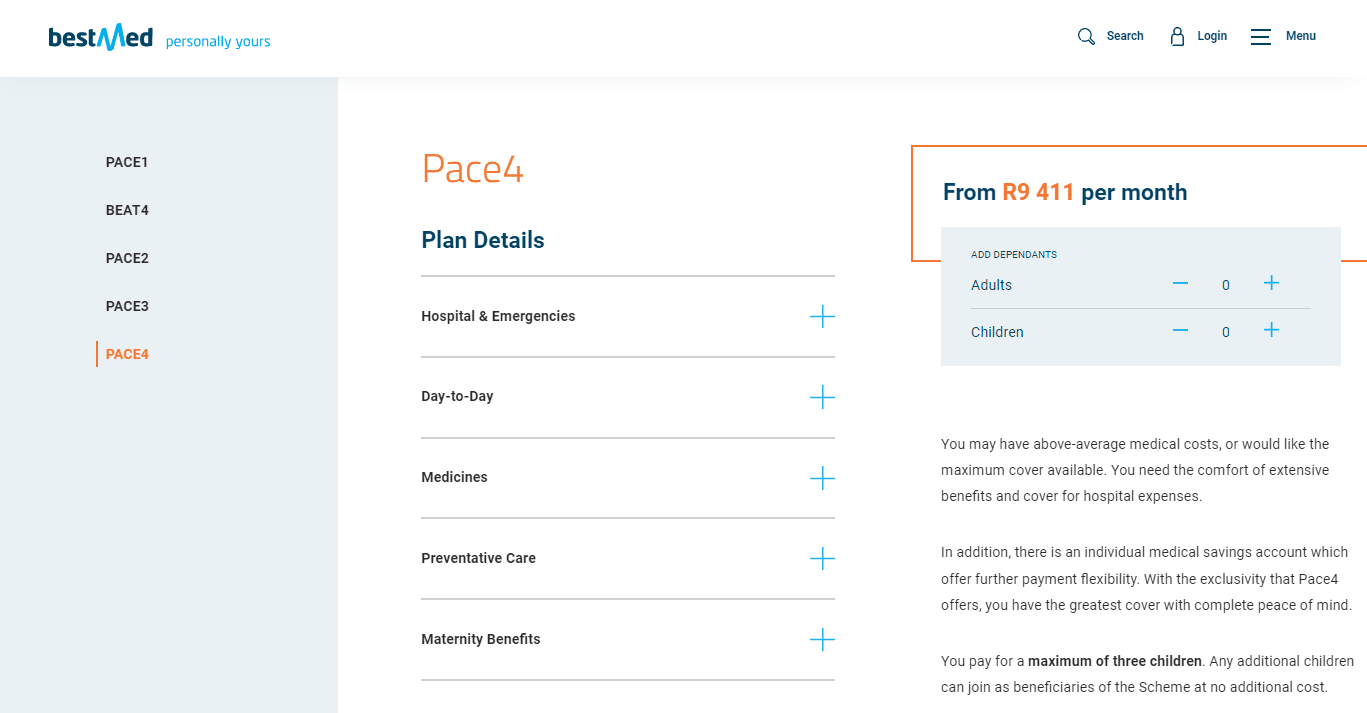
Bestmed Pace 4 Medical Aid Plan
Overall, the Bestmed Pace 4 Medical Aid Plan is a trustworthy and comprehensive medical aid plan that offers 24/7 medical emergency assistance and in-hospital procedures to up to 3 Family Members. The Bestmed Pace 4 Medical Aid Plan starts from R10,343 ZAR.
| 🌎 International Cover | R500,000 – R3 million |
| 👤 Main Member Contribution | R10,343 |
| 👥 Adult Dependent Contribution | R10,343 |
| 💙 Child Dependent Contribution | R2,423 |
| 🔁 Gap Cover | None |
| 🏥 Hospital Cover | Unlimited |
| 💶 Prescribed Minimum Benefits (PMB) | ☑️ Yes |
| 📉 Screening and Prevention | ☑️ Yes |
| ⚕️ Medical Savings Account | ☑️ Yes |
| 🍼 Maternity Benefits | ☑️ Yes |
Bestmed Pace 4 Plan – 11 Key Point Quick Overview
- ☑️ Bestmed Pace 4 Plan Overview
- ☑️ Bestmed Pace 4 Plan Contributions and PMSA
- ☑️ Bestmed Pace 4 Plan Benefits and Cover Comprehensive Breakdown
- ☑️ Bestmed Pace 4 Chronic Condition List
- ☑️ Bestmed Pace 4 Preventative Care
- ☑️ Bestmed Tempo Wellness Program
- ☑️ Bestmed Pace 4 Maternity Care Program
- ☑️ Bestmed Pace 4 Plan Exclusions and Waiting Periods
- ☑️ Bestmed Pace 4 Plan vs. Similar Plans from Other Medical Schemes
- ☑️ Our Verdict on The Bestmed Pace 4 Plan
- ☑️ Bestmed Pace 4 Plan Frequently Asked Questions
Bestmed Pace 4 Plan Overview
The Bestmed Pace 4 medical aid plan is one of 10, starting from R10,343 and includes comprehensive cover, extensive in-hospital benefits, decent overall day-to-day cover, basic and specialized dentistry, and more.
Gap Cover is not available on the Bestmed Pace 4 Plan and according to the Trust Index, Bestmed has a trust rating of 3.5.
Bestmed Pace 4 Plan Contributions and PMSA
Monthly Contributions
| 👤 Main Member | 👥 +1 Adult Dependent | 💙 +1 Child Dependent |
| R10,343 | R10,343 | R2,423 |
Medical Savings Account Available at the start of the year
| 👤 Main Member | 👥 +1 Adult Dependent | 💙 +1 Child Dependent |
| R310 x 12 Months | R310 x 12 Months | R73 x 12 Months |
Bestmed Pace 4 Plan Benefits and Cover Comprehensive Breakdown
Pace 4 Comprehensive Cover for in and out-of-hospital
Savings Account / Day-to-day Benefits:
- ✅ There is a savings account available.
- ✅ There are limited day-to-day benefits offered.
You might consider: 10 Best Hospital Plans in South Africa
Bestmed Pace 4 In-Hospital Benefits
Method of Payment on Pace 4 Plan
- ✅ On the Pace4 option, Scheme risk is used to pay for in-hospital, out-of-hospital, and preventative care benefits.
- ✅ Once the out-of-hospital risk benefits have been depleted, additional claims will be paid from the savings.
While engaging designated service providers, all benefits for conditions that meet the requirements for PMBs will be covered (DSPs). Furthermore, this will not impact your savings (annual or vested).
Bestmed Pace 4 Scheme Benefits for Different Medical Events In-Hospital
- ✅ Members must get pre-approval for all planned operations at least fourteen (14) days before the event. In emergencies, however, the member, their authorized representative, or the hospital must notify Bestmed of the member’s hospitalization as soon as feasible or on the first business day after admission.
- ✅ Clinical procedures, preferred providers, designated service providers, formularies, funding rules, and the Mediscor Reference Price (MRP) could apply.
All listed benefits are subject to pre-approval, clinical protocols, and funding guidelines.
| 🔎 In-Hospital Accommodation and fees for the theatre | Covered up to 100% of the Bestmed tariff. |
| 💊 Take-home medication after discharge | Covered up to 100% of the Bestmed tariff. Limited to a 7-day supply. |
| 🏥 Treatment in Mental Health Clinics | Covered up to 100% of the Bestmed tariff. Limited to 21 days per beneficiary yearly. |
| 🧪 Chemical and Substance Abuse Treatment | Covered up to 100% of the Bestmed tariff. Limited to 21 days or R37,352 per beneficiary per year. Subject to members using network facilities. |
| 🩺 Consultations and procedures | Covered up to 100% of the Bestmed tariff. |
| 📌 Surgical Procedures (including anesthetic) | Covered up to 100% of the Bestmed tariff. |
| ❤️ Organ Transplants | Covered up to 100% of the Bestmed tariff. Only PMBs are covered. |
| 😊 Major medical maxillo-facial surgery (Only specified conditions) | Covered up to 100% of the Bestmed tariff. |
| 🚑 In- and Out-of-Hospital Dental and oral surgery | There is a limit of R23,345 per family. |
| 🦵 Prostheses are subject to preferred providers or co-payments, and limits will apply | Covered up to 100% of the Bestmed tariff. There is a limit of p to R155,450 per family. |
| 🦾 Internal Prostheses (Preferred Providers or limits and co-payments will apply) Functional items used must be towards treating or supporting bodily functions | The following sub-limits apply per beneficiary Functional limited to – R42,000 Pacemakers (dual chamber) – R72,438 Vascular – R72,450 Spinal, including artificial discs – R77,732 Drug-eluting stents – R25,886 Mesh – R22,796 Gynecology/Urology – R18,814 Lens Implants (per lens, per eye) – R20,832 Joint replacements: Hip replacement and other major joints – R69,555 Knee replacement – R80,540 Other minor joints – R25,886 |
| ☑️ External prostheses | There is an annual limit of R35,842per family. Members must use a DSP. This benefit will cover artificial limbs but is limited to one limb every 60 months. |
| ✅ Orthopedic and Medical Appliances | Covered up to 100% of the Bestmed tariff. |
| 📌 Pathology | Covered up to 100% of the Bestmed tariff. |
| 📈 Radiology | Covered up to 100% of the Bestmed tariff. |
| 📉 MRI, CT scans, and other specialized diagnostics | Covered up to 100% of the Bestmed tariff. |
| 📊 Oncology | Covered up to 100% of the Bestmed tariff. The benefit is subject to pre-authorization and the use of DSP |
| ➡️ Peritoneal Dialysis and hemodialysis | Covered up to 100% of the Bestmed tariff. The benefit is subject to pre-authorization and the use of DSP |
| 👶 Birthing Confinements | Covered up to 100% of the Bestmed tariff. |
| 🍼 Mammary surgery on a breast cancer patient’s unaffected (non-cancerous) breast | Covered up to 100% of the Scheme price for reconstructive surgery (which may involve symmetrizing, partial or total mastectomy, etc.) on a breast cancer patient’s healthy breast. The benefit is restricted to R40,476 and requires pre-approval. |
| 🚩 Medically required breast reduction surgery (Includes surgeon and anesthesiologist expenses) | Covered up to 100% of the Scheme tariff. There is a limit of R55,493 per family per year (for surgeons and anesthesiologists). The Scheme risk will cover surgical and hospital expenses. This benefit is subject to the funding protocol and pre-approval. |
| ⚕️ HIV/AIDS | Covered up to 100% of the Bestmed tariff. The benefit is subject to pre-authorization and the use of DSP |
| 😷 Refractive Surgery (and all other procedures that aim to improve or stabilize vision, excluding cataracts) | Covered up to 100% of the Bestmed tariff. Subject to pre-approval and other protocols. Covered up to a limit of R11,117 per eye. |
| 💙 Midwife-assisted birth | Covered up to 100% of the Bestmed tariff. |
| 🅰️ Supplementary Services | Covered up to 100% of the Bestmed tariff. |
| 🅱️ Hospitalization Alternatives | Covered up to 100% of the Bestmed tariff. |
| 📌 Palliative and Home-Based Care instead of hospitalization | Covered up to 100% of the Bestmed tariff. There is a limit of R133,182 per beneficiary yearly. Subject to benefit availability, pre-authorization, and treatment plan. |
| 🏥 Day Procedures performed at a day hospital | Funded at 100% of the Network or Scheme Tariffs if DSPs are used. There is a co-payment of R2,625 when voluntarily using a non-DSP specialist or hospital. |
| 🌎 International Travel Cover | Leisure Travel: Cover is limited to 45 days and R500,000 for trips to the United States. All other nations are insured for up to 90 days, and a family (member and dependents) is protected for R3 million. Business Travel to the United States is limited to 45 days and covers up to R500,000. All other nations are insured for up to 45 days, and a family (member and dependents) is protected for R3 million. |
| 🚀 Day Procedures performed at a Day Hospital | Day procedures at DSPs or day hospitals will be reimbursable at the full network or Scheme rate. Voluntary utilization of non-DSP specialists and acute hospitals will incur an R2,500 co-payment. |
Bestmed Pace 4 Out-of-Hospital Benefits
- ✅ Several specified benefits are paid from the annual savings at a 100% Scheme tariff.
- ✅ Once the annual savings account has been drained, payments are paid from Scheme risk at 100% Scheme tariff (limits apply).
- ✅ If you do not spend all the funds in your savings account within five months, they will be moved into a vested savings account and remain your property.
- ✅ Any vested credit in your vested savings account may be used for out-of-hospital expenses not covered by the Scheme or if you have reached your out-of-hospital/day-to-day yearly limit or sub-limits.
- ✅ Clinical financing methods, preferred providers, designated service providers, formularies, funding criteria, and the Mediscor Reference Price (MRP) may be applicable.
- ✅ All planned treatments or procedures must be pre-authorized before administration.
If you have a treatment plan for a Chronic Disease List (CDL) or Prescribed Minimum Benefit (PMB) condition/s, the services in the treatment plan will be paid for first from the applicable day-to-day limit. After the limit has been exhausted, claims will continue to be paid from Scheme risk up to the maximum amount indicated in the treatment plan.
| 🅰️ Overall day-to-day limits | Main Member – R41,472 Main Member + Dependents – R66,878 |
| 🅱️ FP and Specialist Consultations | These consultations are first covered using available funds from the medical savings account. The following limits apply and are subject to the overall day-to-day limit: Main Member – R6,523 Main Member + Dependents – R10,575 |
| 📌 Diabetes Primary Care Consultation | Covered up to 100% of the Scheme price subject to HaloCare registration. Two consultations for primary care at Dis-Chem pharmacies. Paid initially from the “FP and specialist consultations” daily benefit, then Scheme risk. |
| 📍 Basic and Specialized Dentistry | Paid from savings and then from the daily limit. Orthodontics needs pre-approval. The following limits apply to this benefit, subject to the overall day-to-day limit: Main Member – R14,403 Main Member + Dependents – R24,310 |
| 🦷 Orthodontic Dentistry | Covers up to 100% of the Scheme tariff. Subject to pre-approval. The benefit covers up to R12,208 per event for beneficiaries under 18. Subject to the overall daily limit. |
| 🔍 Medical devices, apparatus, appliances | Covered from available savings first. Covered up to 100% of the Bestmed tariff. There is a limit of up to R12,084 per family. This benefit includes repairs to artificial limbs. The benefit is subject to the overall day-to-day limit. |
| 📈 Insulin Pumps (do not include consumables) | Covered up to 100% of the Bestmed tariff. There is a limit of R46,259 per beneficiary every two years. This benefit is subject to pre-approval. |
| 📉 Continuous (CGM) or Flash Glucose Monitoring (FGM) | Covered up to 100% of the Bestmed tariff. There is a limit of R27,746 per family yearly. The benefit is subject to pre-approval. |
| 👩🏻🦼 Wheelchairs | This benefit is limited to R16,342 per family every four years. |
| 🦻 Hearing Aids | Subject to pre-approval. There is a limit of up to R41,746 per beneficiary every two years. Paid up to 100% of the Bestmed tariff. |
| ☑️ Supplementary Services | Covered from available savings first. Limited to the following (subject to overall day-to-day limit): Main Member – R6,523 Main Member + Dependents – R12,839 |
| ✅ Wound Care Benefit (Dressings, negative pressure wound therapy NPWT treatment, and other nursing services Out-of-hospital) | Covered from available savings first. Covered up to 100% of the Bestmed tariff. Limited to R15,930 per family, subject to the overall day-to-day limit. |
| 🤓 Optometry | Benefits are available every 24 months from the last date of service. Network Providers (PPN) Consultations – 1 per beneficiary. Frames are covered up to R1,040 and up to 100% of the cost of standard lenses (single, bifocal, or multifocal), and lens enhancement up to R750. Alternatively, beneficiaries are covered up to R2,375 for contact lenses. Non-Network Providers Consultation – R365 fee when using a Non-Network Provider. Frames are covered up to R780 and: R215 for single-vision lenses. R460 for bifocal lenses. R982.50 for multifocal lenses. R562.50 for lens enhancement. Alternatively, beneficiaries can opt for contact lenses of up to R2,375 |
| 📌 Basic Radiology and Pathology | Covered from available savings first. Subject to the overall day-to-day limit. The following limits apply: Main Member – R6,523 Main Member + Dependents – R12,839 |
| 📍 Oncology | Oncology program at the full Scheme rate. Subject to pre-approval and DSP. Members have access to extended protocols. |
| ✔️ Peritoneal Dialysis and Hemodialysis | Covered up to 100% of the Bestmed tariff. Subject to pre-approval and DSP. |
| ✳️ HIV/AIDS | Covered up to 100% of the Bestmed tariff. Subject to pre-approval and DSP. |
| 📌 MRI scans, CT scans, isotope studies, and PET scans | Maximum of 3 scans allowed per beneficiary per year. 1 PET scan is allowed per beneficiary per year. Scans are subject to pre-approval. |
| 📍 Rehabilitation after a traumatic event | Covered up to 100% of the Bestmed tariff. |
Bestmed Pace 4 Medicine
- ✅ The following benefits may be subject to pre-authorization, clinical protocols, preferred providers (PPs), designated service providers (DSPs), formularies, funding criteria, the Mediscor Reference Price (MRP), and the exclusions listed in Annexure C of the published Regulations.
- ✅ Members will not incur co-payments for PMB pharmaceuticals on the formulary for which no generic substitute exists.
- ✅ Approved PMB biological and non-PMB biological medicine expenses will be paid first from the Biological limit.
After the limit has been depleted, only PMB biological medicine costs will continue to be paid without limit.
| 🔎 CDL and PMB Chronic Conditions | Covered up to 100% of the Bestmed tariff. There is a co-payment of 10% for non-formulary medicine. |
| 📌 Non-CDL Chronic medicine (First paid from the non-CDL limit. After that, approved CDL and PMB medicine is paid from the Scheme Risk) | Twenty-nine conditions are covered. Covered up to 100% of the Bestmed tariff. There is a co-payment of 10% for non-formulary medicine. The following limits will apply: Main Member – R23,000 Main Member + Dependents – R46,209 |
| 📍 Biological medicine | Limited to R569,070 per beneficiary per year. |
| 💊 Other high-cost medication | Covered up to 100% of the Bestmed tariff. |
| 🩺 Acute Medicine | Savings funds are used first, then covered up to (subject to the overall day-to-day-limit): Main Member – R9,809 Main Member + Dependents – R15,237 |
| 🧪 OTC Medication | OTC Medication is subject to available savings funds. |
Bestmed Pace 4 Chronic Condition List
The Bestmed Pace 4 Chronic Condition List and Prescribed Minimum Benefits are as follows:
CDL
- ✅ Addison’s disease
- ✅ Asthma
- ✅ Bipolar Mood Disorder
- ✅ Bronchiectasis
- ✅ Cardiac Failure
- ✅ Cardiomyopathy
- ✅ Chronic obstructive pulmonary disease (COPD)
- ✅ Chronic Renal Disease
- ✅ Coronary Artery Disease
- ✅ Crohn’s Disease
- ✅ Diabetes Insipidus
- ✅ Diabetes mellitus type 1
- ✅ Diabetes mellitus type 2
and many more.
NON-CDL
- ✅ Severe Acne
- ✅ Allergic Rhinitis
- ✅ Alzheimer’s Disease
- ✅ Ankylosing Spondylitis
- ✅ Attention Deficit Disorder (ADD)
- ✅ Attention Deficit Hyperactivity Disorder (ADHD)
- ✅ Autism
- ✅ Blepharospasm
- ✅ Collagen Diseases
- ✅ Dermatomyositis
- ✅ Dystonia
- ✅ Severe Eczema
- ✅ Gastro Esophageal Reflux Disease (GORD)
- ✅ Gout Prophylaxis
- ✅ Hypopituitarism
and many
PMB
- ✅ Aplastic anemia
- ✅ Benign prostatic hypertrophy
- ✅ Cerebral palsy
- ✅ Chronic anemia
- ✅ COVID-19
- ✅ Cushing’s disease
- ✅ Cystic fibrosis
- ✅ Endometriosis
- ✅ Female menopause
and many more.
and maybe read more about Best Medical Aids Cover Pre-Existing Pregnancy
Bestmed Pace 4 Preventative Care
The following benefits could be subject to pre-approval, clinical procedures, preferred providers (PPs), designated service providers (DSPs), formularies, funding guidelines, and the Mediscor Reference Pricing (MRP).
| 🔎 Benefit | ➡️ Gender and Age Group | 📉 Quantity and Frequency | 🔁 Criteria |
| 💉 Flu Vaccines | All | 1 per beneficiary yearly | Applies to all active participants and recipients. |
| 💊 Pneumonia Vaccines | Children <2 Years High-risk adult group | Children – according to the Department of Health Adults – Twice in a lifetime with a booster for beneficiaries 65> | Adults: The Scheme will identify high-risk adults who will be encouraged to receive vaccinations. |
| 🌎 Travel Vaccines | All | Amount and frequency vary by product up to the maximum quantity authorized. | Program risk benefits for mandatory typhoid, yellow fever, tetanus, meningitis, hepatitis, and cholera travel vaccinations. |
| 👶 Baby Growth and Development Assessments | 0 – 2 Years | 3 Assessments per year | Pharmaceutical clinics under the Bestmed Network perform assessments. |
| 🍼 Female Contraceptives | All female beneficiaries of child-bearing age | Depends on the product according to the maximum allowed amount | Annually limited to R2,678 per beneficiary. Covers all items categorized under the female contraception category. |
| 🩺 Intrauterine device (IUD) insertion | All female beneficiaries of child-bearing age | 1 device every 5 years | Consultation and treatment by a gynecologist or family physician. |
| 🧪 HPV Vaccinations | Female Beneficiaries 9 – 26 | 3 vaccines per beneficiary | Vaccinations are funded according to the MRP |
| 📈 Mammogram | All females 40 years> | Once every 2 years | Covered up to 100% of the Bankmed tariff |
| 📉 PSA Screening | Male Beneficiaries | Once every 2 years | It may be performed at a urologist, family practitioner, or network pharmacy clinic. The available savings account covers the consultation fee. |
| 📊 Back and Neck Preventative Care Program | All | Subject to pre-authorization | Providers of choice (DBC/Workability Clinics). This is a prophylactic approach designed to avoid the need for back and neck surgery. The System could discover suitable volunteers. Based on the initial evaluation, a rehabilitation treatment plan is developed and implemented over a period indicated by the provider. This program is an alternative to surgery. |
| ➡️ Pap Smear | Female beneficiaries 18 and older | Once every 24 months | Possible at a gynecologist, family physician, or pharmacy clinic. The consultation will be at the member’s expense. |
Bestmed Pace 4 Preventative Dentistry
The following services may be subject to pre-approval, clinical protocols, and financial guidelines.
| 🔎 Service | 📌 Age | 📍 Frequency |
| 🦷 General full-mouth examination by a general dentist (including the use of gloves and sterile equipment) | 12 years> | Once yearly |
| ☑️ General full-mouth examination by a general dentist (including the use of gloves and sterile equipment) | <12 years | Twice yearly |
| ✅ Full-mouth Intra-Oral Photos | All | Once every 3 years |
| 📈 Intra-Oral Radiograph | All | 2 photos yearly |
| 📉 Scaling or polishing | All | Twice yearly |
| 📊 Fluoride treatment | All | Twice yearly |
| ➡️ Fissure Sealing | Up to and including beneficiaries 21 years old | According to the applicable and accepted protocol |
| 🔁 Space Maintainers | During the primary and mixed denture stage | Once per space |

Bestmed Tempo Wellness Program
The Bestmed Tempo wellness program is designed to assist you in enhancing your health and reaping the benefits that come with it. Therefore, members can access the following advantages:
| ☑️ Temporary Health Assessment (HA) for adults (16 years and older) that includes one of the following per adult beneficiary per year | The Tempo lifestyle questionnaire Blood pressure check Cholesterol check Glucose check Height, weight, and waist circumference These assessments must be conducted at a contracted pharmacy or on-site at employer groups participating in the program. |
| ✅ Bestmed Tempo Fitness and Nutrition Programs (for those older than 16) | Fitness 1 x (face-to-face) fitness assessment with a Tempo partner biokinetics. 1 x (virtual or face-to-face) follow-up discussion to receive a customized fitness/exercise plan from a Tempo partner biokinetics. These fitness benefits are designed to support your Tempo Get Active journey. Nutrition 1 x (in-person) nutrition evaluation with a Tempo partner dietician 1 x follow-up (virtual or in-person) consultation with a Tempo partner dietician to receive your personalized healthy-eating plan. These nutritional benefits are designed to support your Tempo Nutritional Health Journey. |
| ☑️ Emotional wellness journey | Licensed psychologists and healthcare professionals designed this to help you understand and manage your emotions and their impact on your mental health. In addition, this Adventure grants you access to the following: Lifestyle-related knowledge that will assist you in adapting to life’s alterations and surprises. Practical obstacles that will allow you to practice the new abilities you must acquire to evolve from your current emotional and mental state to the state you seek. |
| ✅ Maternity Benefits | Covered up to 100% of the Scheme tariff. Depending on the following benefits: Consultations Nine prenatal consultations with a general practitioner, gynecologist, or midwife. One postnatal consultation with a general practitioner, gynecologist, or midwife. Ultrasounds 1 x 2D ultrasound scan in the first trimester (between 10 and 12 weeks) performed by an FP OR gynecologist OR radiologist. 1 x 2D ultrasound scan in the second trimester (between 20 and 24 weeks) performed by an FP OR gynecologist OR radiologist. Supplements Any item classified as a pregnancy supplement may be claimed up to a monthly limit of R127 for a maximum of nine months. |
Bestmed Pace 4 Maternity Care Program
The Maternity care program is available to pregnant members and their dependents, providing comprehensive services and information. It has been designed with expectant parents’ specific needs and support networks.
READ more: Best Hospital Plans for Pregnancy Coverage
It provides support, education, and advice throughout pregnancy, confinement, and the postnatal period. To access these services, members must register for the Bestmed Maternity care program when they receive confirmation of their pregnancy through a pathology test or scan from their family practitioner or gynecologist.
Once registration is complete, a consultant will reach out to them.
Try our free Ovulation Calculator

Bestmed Pace 4 Plan Exclusions and Waiting Periods
Bestmed Pace 4 Exclusions
Some of the following are excluded from Pace 4. The comprehensive list can be found on the official Bestmed website.
- ✅ Any fees associated with patient and medical staff travel.
- ✅ Medical aids, orthopedic, surgical, and medical appliances, excluding those described in Annexes B.1 to B.4 of the Scheme Regulations and those prescribed for treating specific PMB disorders and available in the public sector.
- ✅ Requested reports, examinations, tests for emigration, immigration, visas, insurance policies, employment, admission to schools and universities, court medical reports, muscle-function tests, fitness examinations and testing, adoption of children, and retirement due to ill health.
- ✅ Any non-functional or cosmetic procedures, operations, or treatments.
- ✅ Accounting for services performed by individuals not registered with the Health Professionals Council of South Africa, the Associated Health Service Professions Board, or a comparable healthcare organization in the nation where the service was rendered.
Unkept appointments by members, and more.
Discover the 5 Best Medical Aids under R2000
Bestmed Pace 4 Waiting Periods
Depending on pre-existing or existing conditions, the following might apply when you register for medical cover with the Bestmed Pace 4 plan:
- ✅ A 3-month general waiting period in respect of all benefits.
- ✅ A 12-month exclusion in respect of a pre-existing condition.
A late-joiner contribution penalty will apply.

Bestmed Pace 4 Plan vs. Similar Plans from Other Medical Schemes
| 🔎 Medical Aid Plan | 🥇 Bestmed Pace 4 | 🥈 Discovery Health Classic Comprehensive | 🥉 LA Health Comprehensive |
| 🌎 International Cover | R500,000 – R3 million | R5 million | R5 million |
| 👤 Main Member Contribution | R10,343 | R8,381 | 9,379 ZAR |
| 👥 Adult Dependent Contribution | R10,343 | R7,927 | 7,161 ZAR |
| 💙 Child Dependent Contribution | R2,423 | R1,671 | 2,274 ZAR |
| 🏥 Hospital Cover | Unlimited | ✅ Yes | Unlimited |
| 💶 Prescribed Minimum Benefits (PMB) | ☑️ Yes | ☑️ Yes | ☑️ Yes |
| 📉 Screening and Prevention | ✅ Yes | ✅ Yes | ✅ Yes |
| ➡️ Medical Savings Account | ☑️ Yes | ☑️ Yes | ☑️ Yes |
| 🍼 Maternity Benefits | ✅ Yes | ✅ Yes | ✅ Yes |

Our Verdict on The Bestmed Pace 4 Plan
Overall, Bestmed’s Pace 4 option is the most comprehensive plan available, designed to provide maximum coverage for hospital expenses and extensive benefits for individuals and families with high medical costs.
It is important to note that Pace 4 requires a higher contribution towards medical coverage, making it a suitable option for families who prioritize peace of mind and are willing to invest in comprehensive medical coverage.
Overall, Bestmed’s Pace 4 plan offers extensive benefits and coverage for families who require above-average medical care.
You might also consider the following options BestMed has to offer:
- ✅ BestMed Beat 3 Network
- ✅ BestMed Beat 2 Network
- ✅ BestMed Beat 1 Network
- ✅ BestMed Tempo
- ✅ BestMed Pace 3
- ✅ BestMed Pace 2
- ✅ BestMed Pace 1
- ✅ BestMed Rhythm 2
- ✅ BestMed Rhythm 1
- ✅ BestMed Beat 4
- ✅ BestMed Beat 3
- ✅ BestMed Beat 2
- ✅ BestMed Beat 1
Frequently Asked Questions
What does Bestmed Pace 4 offer?
Bestmed Pace 4 is the most comprehensive plan offered by Bestmed, providing maximum cover for hospital expenses and extensive benefits for individuals and families with high medical costs.
Is maternity covered under Bestmed Pace 4?
Yes, maternity is covered under Bestmed Pace 4. The scheme covers prenatal consultations, ultrasound scans, childbirth, and postnatal care.
What kind of medical costs does Bestmed Pace 4 cover?
Bestmed Pace 4 is suitable for families with above-average medical costs and who want peace of mind knowing they are fully covered for hospital and day-to-day medical expenses.
Does Bestmed Pace 4 cover oncology treatment?
Yes, Bestmed Pace 4 does cover oncology treatment. The scheme covers cancer treatment in and out of the hospital, including chemotherapy, radiotherapy, and surgical procedures.
How is Bestmed Pace 4 different from other Pace plans?
Unlike other plans in the Pace category, the Family practitioner, Specialist Consultations, and Basic and Specialized Dentistry in the Pace 4 plan are not paid from the savings account but are allocated a limited amount subject to day-to-day benefits.
What are day-to-day benefits?
Day-to-day benefits include out-of-hospital medical expenses such as GP visits, medication, and pathology tests. In the Pace 4 plan, the day-to-day benefits cover Family practitioners, Specialist Consultations, and Basic and Specialized Dentistry.
What is the contribution required for Bestmed Pace 4?
Bestmed Pace 4 requires a higher contribution than other plans due to its more comprehensive coverage. It is designed for families willing to invest in comprehensive medical coverage.
What are the advantages of choosing Bestmed Pace 4?
Bestmed Pace 4 offers extensive benefits and coverage for families who require above-average medical care. In addition, it provides peace of mind knowing that individuals and families are fully covered for hospital and day-to-day medical expenses.
Does Bestmed Pace 4 cover alternative therapies such as acupuncture or homeopathy?
No, Bestmed Pace 4 does not cover alternative therapies such as acupuncture or homeopathy.
Does Bestmed Pace 4 cover dental procedures?
Yes, Bestmed Pace 4 covers basic and specialized dentistry, subject to overall limits and protocols.
Does Bestmed Pace 4 cover over-the-counter medication?
No, Bestmed Pace 4 does not pay for OTC medication. Instead, OTC medication is covered by the available medical savings account. Furthermore, if the medical savings are depleted, members are responsible for paying medication out-of-pocket.
Does Bestmed Pace 4 cover ambulance services?
Yes, Bestmed Pace 4 covers emergency ambulance services that are medically necessary.
You might also like
Table of Contents
Free Medical Aid Quote
Our Trusted Partners
We work with leading medical aid companies in South Africa.

7 Actionable Ways to save 32% on your MEDICAL AID in 14 days.

- +27 72 7967 530
- [email protected]
- 2nd Floor, West Tower, Nelson Mandela Square, Sandton, 2196, Johannesburg, Gauteng, South Africa
🔎 Report a bug or outdated data to be updated to [email protected]
© Medicalaid.com | All rights Reserved |
Copyright 2024
Top 5 Medical Aids
Top 5 Gap Cover Plans
































