- Medical Aid
- Currently Trending
The Best Medical Aids
- Compare Plans
- Gap Cover
- Best Gap Covers
- Hospital Plans
- Currently Trending
The Best Hospital Plans
- Medical Insurance
- Pet Insurance
Medihelp MedElect Medical Aid Plan
Overall, the Medihelp MedElect Medical Aid Plan is a trustworthy and comprehensive medical aid plan well suited to both suited to students and families offering 24/7 medical emergency assistance and care extender benefits. The Medihelp MedElect Medical Aid Plan starts from R984 for MedElect Student.
| 👤 Main Member Contribution | R894 – R2,820 |
| 👥 Adult Dependent Contribution | R894 – R2,208 |
| 🍼 Child Dependent Contribution | R894 – R912 |
| 📉 Annual Limit | Unlimited Hospital Cover |
| 🏥 Hospital Cover | Unlimited |
| 🏠 Home Care | ☑️ Yes |
| 💶 Prescribed Minimum Benefits | ☑️ Yes |
| 💻 Screening and Prevention | ☑️ Yes |
| 💳 Medical Savings Account | None |
| 🦷 Advanced Dentistry | ☑️ Yes |
Medihelp MedElect Plan – 10 Key Point Quick Overview
- ☑️ Medihelp MedElect Plan Overview
- ☑️ Medihelp MedElect Plan Contributions
- ☑️ MedElect Plan Benefits and Cover Comprehensive Breakdown
- ☑️ MedElect Hospitalization and Advanced Treatment
- ☑️ MedElect Emergency Benefits
- ☑️ MedElect Added Insured Benefits
- ☑️ Medihelp MedElect Plan Exclusions and Waiting Periods
- ☑️ Medihelp MedElect Plan vs. Similar Plans from other Medical Schemes
- ☑️ Our Verdict on The MedElect Plan
- ☑️ MedElect Plan Frequently Asked Questions
Medihelp MedElect Plan Overview
The Medihelp MedElect medical aid plan is one of 11, starting from R894, and includes cover for students, several day-to-day benefits for the entire family, care extender benefits, optometry, dentistry, and more. Gap Cover is not available on the Medihelp MedElect Plan. However, Medihelp offers 24/7 medical emergency assistance. According to the Trust Index, Medihelp has a trust rating of 4.2.
MediHelp has the following 11 plans to choose from
- ✅ MediHelp Medprime
- ✅ MediHelp MedPrime Elect
- ✅ MediHelp MedPlus
- ✅ MediHelp MedElite
- ✅ MediHelp MedVital
- ✅ MediHelp MedVital Elect
- ✅ MediHelp MedSaver
- ✅ MediHelp MedMove
- ✅ MediHelp MedElect
- ✅ MediHelpMedAdd
- ✅ MediHelp MedAdd Elect
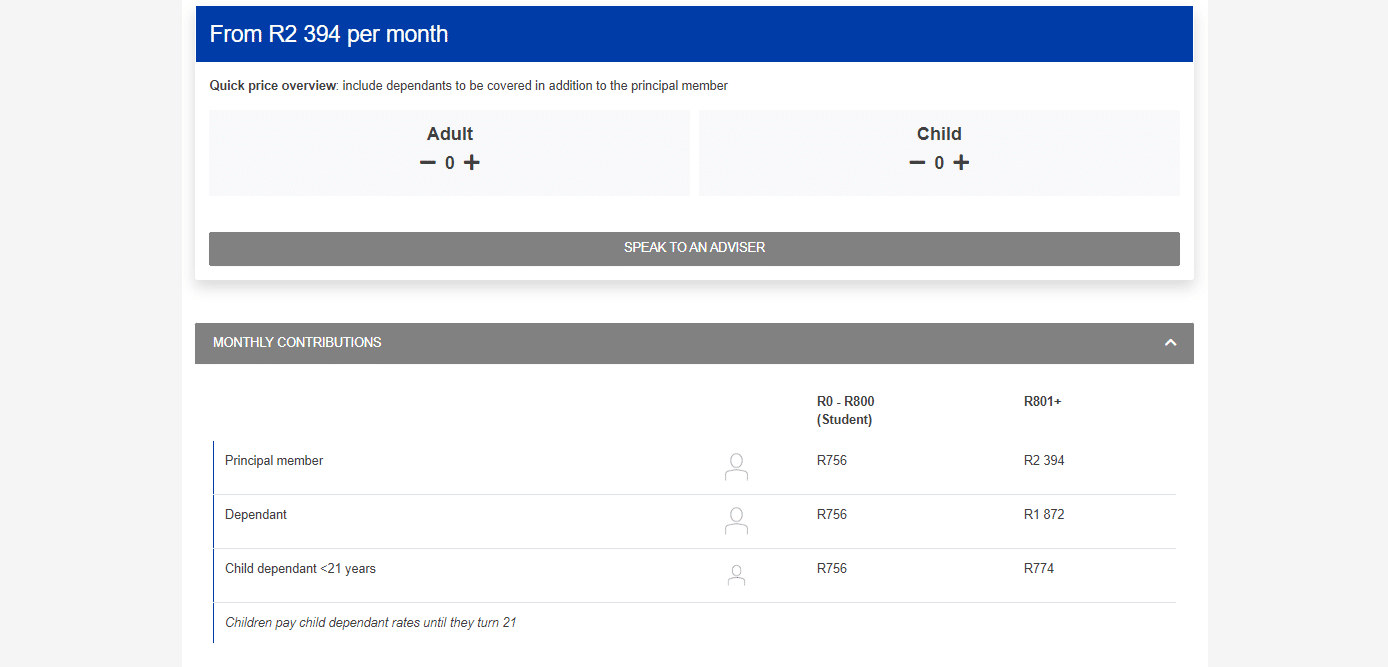
Medihelp MedElect Plan Contributions
Contributions for Students
| 👤 Main Member | 👥 +1 Adult Dependent | 💙 +1 Child Dependent |
| R894 | R894 | R894 |
Read more about:
Contributions for Other Members
| 👤 Main Member | 👥 +1 Adult Dependent | 💙 +1 Child Dependent |
| R2,820 | R2,208 | R912 |
MedElect Plan Benefits and Cover Comprehensive Breakdown
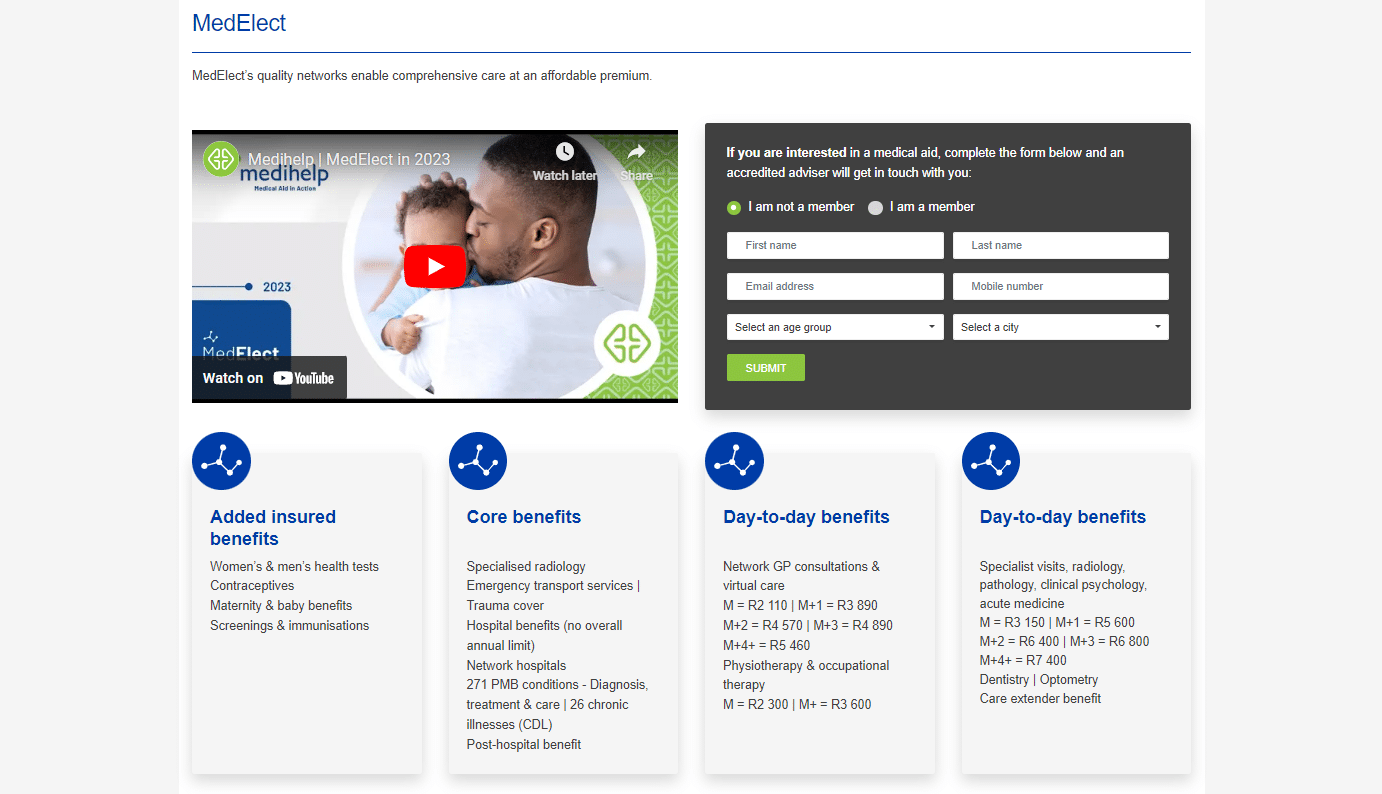
MedElect Day-to-Day Benefits
Paid up to 100% of the Medihelp Tariff (MT). The following is available for day-to-day medical expenses:
- Main Member – R3,150 per year
- Main Member +1 Dependent – R5,600 per year
- Main Member +2 Dependents – R6,400 per year
- Main Member +3 Dependents – R6,800 per year
- Main Member +4 Dependents = R7,400 per year
The following is paid from day-to-day benefits:
- Specialists’ services upon referral by a network Physician and pre-authorization according to Medihelp’s standards, with the proviso that the authorization for the initial expert consultation includes one follow-up appointment. Specialist services incur a 35% co-payment in case of no reference, referral by a non-network Doctor, and absence of prior authorization.
- Basic radiology and pathology. Pathology DSPs applicable (Ampath)
- Clinical psychology services on referral by a network Physician. If there is no referral, referral by a non-network GP, or referral by a specialist when the specialist’s services have not been pre-authorized, a 35% co-payment on the benefit amount is required.
Acute and non-PMB chronic medicine (prescribed or issued by a network Doctor and obtained from a network pharmacy). 20% co-payment if not purchased from a network pharmacy or prescribed by a network physician.
- Generic medication – 100% of the MMAP
- Original drug if no generic equivalent is available – 80% of the MT
- The original drug used voluntarily when a generic equivalent is available – 70% of the MMAP
POLL: 5 Best Medical Aids under R300
MedElect Day-to-Day Benefit Table
| 💊 Self-Medication | Covered up to 100% of the MT. Subject to the annual day-to-day benefit with the following limits: Main Member – R560 per year Main Member + Dependents – R1,650 per year |
| 💉 PMB Chronic Medicine | Pre-approval and registration on Medihelp’s PMB drug management program are required. Covered up to 100% of the MHRP. The unlimited cover is provided. There is a 30% co-payment if services are obtained from a non-network pharmacy or dispensing GP. |
| Consultations and follow-up Consultations | Surgical and medical services, in addition to anesthesia Material and discretionary medicine used during the performance of a service, except chronic disease vaccinations and immunizations. Covered up to 100% of the MT, but the following limits apply: Main Member – R2,110 per year Main Member + 1 – R3,890 per year Main Member + 2 – R4,570 per year Main Member + 3 – R4,890 per year Main Member + 4 – R5,460 per year |
| 👩⚕️ Consultations: Virtual Care by GPs and Nurses | Surgical and medical services, in addition to anesthesia Material and discretionary medicine used during the performance of a service, except chronic disease vaccinations and immunizations. Covered up to 100% of the MT, but the following limits apply: Main Member – R2,110 per year Main Member + 1 – R3,890 per year Main Member + 2 – R4,570 per year Main Member + 3 – R4,890 per year Main Member + 4 – R5,460 per year |
| 👨⚕️ Out-of-Network GP Consultations Consultations, follow-ups, and emergency unit visits Surgery and anesthesia Material and discretionary medicine used during service, except vaccines/medicine for chronic conditions and immunizations. | Covered up to 80% of the MT Limited to R1,300 per year for the main member and up to R2,600 for the main member plus beneficiaries. |
| 🚑 Other Medical Services in and Out-of-Hospital Physiotherapy Occupational Therapy | Covered up to 100% of the MT Limited to R2,300 for the main member and R3,600 for the main member and dependents per year. There is a 35% co-payment if the following applies: The physiotherapy and occupational therapy account either does not include the referring doctor’s office number or lists an out-of-network doctor’s office. The account lists a non-pre-authorized specialist’s practice number. |
| 🔁 Care Extender: Additional GP Consultation | A beneficiary’s Pap smear, mammography, prostate test, FOBT, or bone mineral density test activates a family consultation benefit. |
| ➡️ Care Extender: R475 for Self-Medication | After a beneficiary claims the combo health screening (blood glucose, cholesterol, BMI, and blood pressure measurement) at a preferred pharmacy clinic, the family will receive R475 for non-prescribed medicine. |
| 🔎 Care Extender: Oxygen | Covered up to 100% of the MT. Unlimited cover. A 35% co-payment applies if not authorized. |
| 🤓 Optometry | Subject to pre-authorization by a PPN. Services must be via a PPN provider. There is a limit of 1 composite consultation, including refraction test, tonometry, and visual field test per 2-year cycle. Covered up to 100% of the MT. |
| 👓 Spectacles or Contact Lenses | Spectacles – Frames or lens enhancement Limited to R565 per beneficiary/2 years. Lenses (1 x clear pair) Limited to single-vision or bifocal lenses per beneficiary/2 years. Multifocal lenses are covered at the cost of bifocal lenses. Contact lenses Limited to R775 per beneficiary/2 years. |
| 🦷 Conservative Dental Services | Benefits are subject to Dental Risk Company (DRC) protocols, contracted to Medihelp as a DSP. Benefits are subject to protocols and are limited to certain item codes. |
| 🪥 Dentistry: Routine Check-ups | Covered up to 100% of the MT. Limited to one check-up per beneficiary per year or per 6-month cycle. |
| 😊 Oral Hygiene | Scale and Polish Treatments: Covered up to 100% of the MT. Limited to one check-up per beneficiary per year or per 6-month cycle. Fluoride Treatment for children between 5 and 13: Covered up to 100% of the MT. Limited to one treatment per beneficiary per year or a 6-month cycle. Fissure sealants for children between 5 and 16 (permanent teeth): Covered up to 100% of the MT. |
| 📌 Dentistry: Fillings | Treatment plans and x-rays might be requested where multiple fillings are necessary. Covered up to 100% of the MT. Limited to 4 fillings per beneficiary yearly or one filling per tooth in one year. |
| 📍 Tooth Extractions and Root Canals on permanent teeth in the Dentist’s chair | Covered up to 100% of the MT. |
| 🙂 Laughing Gas (Dentist’s Chair) | Covered up to 100% of the MT. |
| ☑️ Dentistry under conscious sedation (Dentist’s chair) | The benefit is only available for removing impacted teeth (3rd molars) Covered up to 100% of the MT 35% co-payment for no authorization. |
| 💤 Dentistry under general anesthesia in a day procedure facility, including the removal of impacted teeth | Covered up to 100% of the MT 35% co-payment for procedures not performed in a day procedure network. 20% co-payment for no authorization. |
| 🚩 Extensive dental treatment for children <7 (only once per beneficiary yearly) | Covered up to 100% of the MT 20% co-payment for no authorization. Covered from the savings account. |
| ✳️ Special Needs Patients – dentistry under general anesthesia in a day procedure | Covered up to 100% of the MT 35% co-payment for procedures not performed in a day procedure network. 20% co-payment for no authorization. |
| 🅰️ Plastic Dentures | Covered up to 80% of the MT. Limited to one set every 2 years for beneficiaries 21> |
| 🅱️ X-Rays | Intra-Oral X-Rays Covered up to 100% of the MT. Limited to 4 per beneficiary yearly. Extra-Oral X-Rays Covered up to 100% of the MT. Limited to one per year every three years. |
| 🔁 Specialized Dentistry | Covered up to 100% of the MT. |
| 😊 Maxillofacial Surgery and Oral Pathology | Only PMBs are covered Subject to pre-approval by Medihelp and the necessary clinical protocols. |
| 🦵 External Prostheses and Medical Appliances Services in and out of the hospital, including fitting, cost of repairs, maintenance, spares, accessories, and adjustments on the following: Wheelchairs Medical Appliances Glucometers every 5 years. | Covered up to 100% of the MT. Limited to R1,050 per family per year. |
| 🦾 External Prostheses and Medical Appliances Stoma Components Incontinence Products or Supplies | Covered up to 100% of the MT. Unlimited cover. |
Try our: Free medical aid compare tool.
MedElect Hospitalization and Advanced Treatment
| 💊 Chronic Illness and PMB | Subject to protocols, pre-authorization, DSPs, and the specialist network. Covered up to 100% of the cost or the contracted tariff. Unlimited cover provided. Co-payments can apply if not using a DSP or deviating from the code. |
| ⚠️ Trauma Benefits This applies to major trauma requiring hospitalization, for example: Motor Vehicle Accidents Stab Wounds Gunshot Wounds Head Trauma Burns Near-drowning | Subject to authorization, PMB protocols, and case management. Covered up to 100% of the cost or the contracted tariff. |
| 😷 Post-Exposure Prophylaxis (HIV/AIDS) | Subject to authorization, PMB protocols, and case management. Covered up to 100% of the cost or the contracted tariff. |
| 🚑 Emergency Transport Services via Netcare 911 In the Beneficiary’s Country of Residence (RSA, Lesotho, Eswatini, Mozambique, Namibia, Zimbabwe, Botswana), including road and air transport. | Unlimited Cover. Covered up to 100% of the MT. If not pre-approved, a 50% co-payment applies. |
| 🏥 Emergency Transport Services via Netcare 911 Outside the beneficiary’s Country of Residence | Road Transport Covered up to 100% of the MT. If not pre-approved, a 50% co-payment applies. Limited to R2,320 per case. Air Transport Covered up to 100% of the MT. If not pre-approved, a 50% co-payment applies. Limited to R15,400 per case. |
| ➡️ Hospitalization (Only MedElect hospital and day procedure network can be used): Intensive Care and high-care wards Ward Accommodation Theatre fees Treatment and medicine in the ward In-hospital consultation with GPs and specialists Surgery Anesthesia | Unlimited Cover. Covered up to 100% of the MT. If not pre-approved, a 20% co-payment applies. A 35% co-payment will apply if members are admitted to non-network hospitals or day facilities. Additional co-payments on certain procedures may apply. |
| ✳️ Hospitalization (Only MedElect hospital and day procedure network can be used): Day Procedures (Including Ophthalmological, endoscopic, ear, nose, and throat procedures, dental procedures, removal of skin lesions, circumcisions, and procedures as pre-authorized) | Unlimited Cover. Covered up to 100% of the MT. If not admitted to a hospital/day procedure facility in the network, a 35% co-payment applies. Additional co-payments on certain procedures may apply. |
| 🅰️ Hospitalization (Only MedElect hospital and day procedure network can be used): Hospital Medicine upon Discharge | Covered up to 100% of the MT. There is an R390 limit per admission. |
| 🏠 Home Delivery Includes the following: Professional Nursing Fee Equipment Material and Medicine | Covered up to 100% of the MT. Limited to R14,900 per event. If not pre-approved, a 20% co-payment applies. |
| 📈 Radiography | Covered up to 100% of the MT. Limited to R1,210 per family yearly. |
| 📉 Specialized Radiography | MRI and CT scans Subject to pre-authorization. Covered up to 100% of the MT. Unlimited Cover. Member pays the first R3,300 per examination and R2,800 out of the hospital. Benefits do not apply if treatment is not pre-approved. Angiography Covered up to 100% of the MT. Unlimited Cover. Benefits do not apply if treatment is not pre-approved. |
| 📊 Clinical Technologist Services | Covered up to 100% of the MT. Unlimited Cover. |
| ❤️ Organ Transplants | Covered up to 100% of the MT. Unlimited Cover. Subject to pre-authorization and clinical protocols. Cornea implants Covered up to 100% of the MT. Limited to R32,600 per implant yearly. |
| ⚕️ In-hospital Oxygen | Covered up to 100% of the MT. Unlimited Cover. |
| 🔎 Renal Dialysis Acute Renal Dialysis Chronic/Peritoneal Renal Dialysis | Covered up to 100% of the MT. Unlimited Cover. Subject to pre-authorization and clinical protocols. 20% co-payment if not pre-approved. |
| 🔍 Post-Hospital Care Speech therapy, occupational therapy, and physiotherapy 30 days after discharge | Accessible day-to-day benefits cover prescription medication and medical equipment. Covered up to 100% of the MT. Limited to the following: Main Member – R2,100 per year. Main Member + Dependents – R3,000 per year. |
| 📌 Other Medical Services Dietitian services, physiotherapy, and occupational therapy Speech therapy Audiometry and orthoptic services Podiatry | In-hospital protocols might apply. Covered up to 100% of the MT. Unlimited Cover. |
| 📍 Physiotherapy and Occupational therapy | Pre-approval required. An attending doctor must request it. Covered up to 100% of the MT, but these limits apply: Main Member – R2,300 per year. Main Member + Dependents – R3,600 per year. |
| ☑️ Psychiatry Psychiatrist-provided hospital and outpatient treatments General ward accommodations Institution-supplied medication Outpatient consultations | Covered up to 100% of the MT. Limited to R21,840 per beneficiary per year, with a limit of R33,180 per family per year. A co-payment of 35% applies if a member voluntarily goes to a non-network hospital, if a GP or Specialist does not request treatment, or if requested by a specialist with no approved referral by a GP in the network. If not pre-approved, a 20% co-payment applies. |
| Oncology: PMB Cases | Pre-authorization and Medihelp Oncology Program registration are required. Protocols, a DSP, and the MORP apply. Covered up to 100% of the MT. Unlimited Cover. 10% co-payment on non-DSP treatment. 25% co-payment for deviating from protocol. |
| ✅ Oncology: Non-PMB Cases | Covered up to 100% of the MT. Limited to R231,000 per family per year. 10% co-payment on non-DSP treatment. 20% co-payment for deviating from protocol. If there is a deviation from the protocol, the benefit does not apply. |
| 💊 Alternative Hospitalization Services: Hospice Services and Subacute Care Facilities | Covered up to 100% of the MT. 20% co-payment if not pre-authorized Limited to R25,400 per family per year. A 35% co-payment applies for private nursing services without pre-authorization. |
| 💉 Alternative Hospitalization Services: Palliative Care | Covered up to 100% of the MT. 20% co-payment if not pre-authorized Limited to R19,800 per family per year. |
| 😷 Alternative Hospitalization Services: Private Nursing | Covered up to 100% of the MT. 20% co-payment if not pre-authorized Limited to R25,400 per family per year. A 35% co-payment applies for private nursing services without pre-authorization. |
| 📌 Appendectomy: Conventional or Laparoscopic Procedure | Unlimited cover. Covered up to 100% of the MT. |
| 📍 Prostatectomy: Conventional or Laparoscopic Procedure | Member pays the first R7,200 per admission. Covered up to 100% of the MT. |
MediHelp MedElect Childbirth
Subject to pre-authorization, protocols, and case management
- Unlimited Cover.
- Covered up to 100% of the MT.
- If not pre-approved, a 20% co-payment applies.
- A 35% co-payment applies when voluntarily using a non-network hospital.
Discover the 5 Best Medical Aids for Pregnant Women
Radiology, Pathology, and Medical Technologist Services
- In-Hospital cover only.
- Covered up to 100% of the MT.
- Unlimited cover provided.
- Subject to clinical protocols and approved hospital admission.
- Members must use Ampath as the contracted Pathology DSP.
MedElect Emergency Benefits
A medical emergency is a sudden and unexpected occurrence that necessitates quick medical or surgical treatment to safeguard a patient’s health. Failure to offer medical or surgical treatment would result in severe impairment of bodily functioning or severe dysfunction of a bodily organ or portion or jeopardize the individual’s life. Netcare 911 is the designated service provider for Medihelp’s emergency transport services, and you must contact them in an emergency. Phone 082 911. Furthermore, you may also seek assistance at the nearby hospital’s emergency room. However, the following conditions apply:
- Emergency admissions must be reported to Medihelp on the following business day by calling 086 0200 678.
- If you visit an emergency facility but are not hospitalized, the care you receive will be covered by your regular plans.
- Facilities costs are not included.
| 🚑 In the Beneficiary’s Country of Residence | Unlimited Cover. Covered up to 100% of the MT. If not pre-approved, a 50% co-payment applies. |
| 🚑 Outside the beneficiary’s Country of Residence | Road Transport: Covered up to 100% of the MT. If not pre-approved, a 50% co-payment applies. Limited to R2,320 per case. Air Transport: Covered up to 100% of the MT. If not pre-approved, a 50% co-payment applies. Limited to R15,400 per case. |
You might like to know about the 5 Best Hospital Plans under R300
MedElect Added Insured Benefits
- With a strong emphasis on preventative care, early diagnosis of potential health problems, and maternity benefits and childcare, these benefits are offered annually in addition to your insured benefits unless otherwise specified.
- Protocols and item codes may be applicable.
- Members can look for network provider information on Medihelp’s website or app using the provider search option.
- You can also sign up for HealthPrint, a free online health and fitness program offered by Medihelp, to activate the specified benefits.
| ☑️ Mammogram | For women 40 – 75 years old. Every two years. A medical doctor must request it. |
| ✅ Pap Smear | For women 21 – 65 years old. Every three years. A medical doctor must request it. |
| ☑️ Flu Vaccines | Once yearly. It must be done at network pharmacy clinics. |
| ✅ Contraceptives | Oral, injectable, or implantable contraceptives Female beneficiaries up to 50 years. Covered up to R150 per month and up to R1,950 per beneficiary. Intra-uterine devices for women up to 50 years Every 60 months. Covered up to R2,200 per beneficiary. |
| ☑️ Enhanced Maternity Benefits HealthPrint’s Maternity and Infant program registration will activate these additional benefits per family per year. | Ten prenatal and postnatal consultations with a midwife, general practitioner, or gynecologist. However, a recommendation from a network GP to the gynecologist is not required. Two prenatal and postnatal visits to a lactation consultant, dietician, or antenatal classes. Two 2D ultrasound imaging. |
| ✅ Child Benefits | Babies <2 years receive two additional visits to a general practitioner, pediatrician, or ear, nose, and throat specialist. However, a network Physician reference is not required to see these specialists. In network pharmacy clinics, the full series of regular child immunizations are covered for up to seven years. Vaccination of children against influenza at network pharmacy clinics. |
| ☑️ Routine Screening and Immunization | A combo test, including blood glucose, cholesterol, BMI & blood pressure measurement. Individual tests, including blood glucose or cholesterol. HIV testing, counseling & support A tetanus vaccine A flu vaccination Two HPV vaccinations for girls and boys between 10 – 14 years or three between 15 – 26 years |
| ✅ Men’s Health | A prostate test (PSA level) was requested by a physician for men aged 40 to 75. Flu vaccination is administered at network pharmacies. |
| ☑️ Screening and Immunization for beneficiaries 45> | An FOBT test for recipients 45-75 years Women aged 65 and older can access one bone mineral density test every two years if requested by a physician. A Pneumovax vaccine on a 5-year cycle for each 55-year-old with asthma or COPD who is registered. |
| ✅ Wellness Support | Back Treatment – this benefit covers back therapy at a DBC facility as an alternative to surgery for eligible patients. Moreover, treatment is a precondition for spinal surgery. One dietitian consultation with each registered HealthPrint member whose BMI is greater than 30 and whose BMI was determined by a BMI test. An oncology schedule is provided in conjunction with Independent Clinical Oncology Network oncologists (ICON) HIV program – Presented in partnership with LifeSense Disease Management |
| ☑️ Care Extender Benefit | Additional GP visit Once your increased insured benefits pay for a Pap smear, mammography, prostate test, FOBT, or bone mineral density test, the family will receive a one-time GP visit benefit. Test protocols will apply to this benefit. Self-Medication (R475) Once your enhanced insured benefits pay for a combo health screening (blood glucose, cholesterol, BMI, and blood pressure), the family will receive a one-time R475 for self-medication. |
Medihelp MedElect Plan Exclusions and Waiting Periods
Medihelp MedElect Exclusions
As medical research advances, new medical services are introduced each year. However, Medihelp covers life-saving medical treatment first. The Medical Schemes Act requires medical schemes to cover the diagnostic, treatment, and care costs of the mandated minimum benefits (PMB) without co-payments or limits. Furthermore, services must follow legislation’s PMB treatment algorithms and Medihelp’s managed healthcare guidelines, which may include pharmaceutical formularies. Medihelp will cover the cost of a substitute treatment if a protocol or formulary drug is ineffective or hazardous. However, the Medihelp MedElect plan excludes several items, including but not limited to the following.
- The treatment of infertility other than that specified in the Medical Schemes Act of 1998 Regulations
- The artificial insemination of a human, as defined in section 61 of the National Health Act of 2003
- Immunizations (including immunization processes and materials) required by an employer, excluding flu vaccinations and routine childhood immunizations
- Workout, coaching, and rehabilitation regimens
- The cost of extracting or conserving human tissues, including but not limited to stem cells, for future use in the treatment of an undiagnosed medical ailment in a beneficiary
- Pathology services requested by someone other than a physician
- Non-registered substances with the South African Health Products Regulatory Authority (SAHPRA).
- This does not apply to medicines exempted by section 21 of the Medicines and Related Substances Control Act (101 of 1965, as amended)
- Bandages, cotton wool, bandages, plasters, and similar items not utilized by a service provider during a treatment or procedure
- Food substitutes, food supplements, and prescription food, including infant food.
- Multivitamin and multimineral supplements alone or with stimulants (tonics)
- Appetite suppressants
- Cost of metal-based complete dentures, including laboratory fees
- Impact-resistant acrylic
- The expense of gold, precious metal, semi-precious metal, and platinum foil
- Laboratory delivery fees
- Blood pressure apparatus
- Commode
- Toilet seat raiser
- Home-use hospital beds
- Devices to improve vision, other than the stated eyeglass and contact lens benefits
POLL: 5 Best Medical Aid with Immediate Cover (No Waiting Period)
Medihelp MedElect Waiting Periods
During waiting periods, members are eligible for membership but not for benefits. For example, Medihelp could implement either a general or condition-specific waiting period as follows:
- The general waiting period is up to three months from the date of membership. During this time, you will not be eligible for benefits other than the minimum prescribed benefits (PMB). During this waiting period, the Scheme will not pay any claims you file.
- From the day you join, a condition-specific waiting period of up to 12 months applies. During this period, you will not be eligible for benefits related to a specific ailment for which you get medical advice, a diagnosis, care, or treatment (this excludes PMB).
Medihelp MedElect Plan vs. Similar Plans from other Medical Schemes
| MediHelp MedElect | Discovery KeyCare | Bonitas BonEssential | |
| 🌎 International Cover | None | TBC | TBC |
| 👤 Main Member Contribution | R894 – R2,880 | R1,102 – R3,354 | R2,287 |
| 👥 Adult Dependent Contribution | R894 – R2,880 | R1,102 – R3,354 | R1,690 |
| 💙 Child Dependent Contribution | R894 – R912 | R664 – R 897 | R739 |
| 📉 Annual Limit | Unlimited Hospital Cover | None | Several limits and sub-limits |
| 💶 Prescribed Minimum Benefits (PMB) | ✅ Yes | ✅ Yes | ✅ Yes |
| 📊 Screening and Prevention | ☑️ Yes | ☑️ Yes | ☑️ Yes |
| 💳 Medical Savings Account | None | None | ✅ Yes |
| 🍼 Maternity Benefits | ✅ Yes | ✅ Yes | ✅ Yes |
| 🏠 Home Care | ☑️ Yes | ☑️ Yes | ☑️ Yes |
Our Verdict on The MedElect Plan
Medihelp’s MedElect plan is a comprehensive medical aid plan that offers its members a wide range of benefits. One of the standout features of this plan is its unlimited hospital cover, which means that members are covered for all hospital-related expenses, including accommodation, theatre, and specialist fees. In addition, the plan offers generous benefits for chronic medication. Furthermore, it covers day-to-day medical expenses such as GP consultations, dentistry, and optometry.
One of the drawbacks of the MedElect plan is that it is relatively expensive compared to other Medihelp plans and may not be suitable for individuals or families on a tight budget. Additionally, the plan may not offer as much flexibility or customization options as some other plans offered by Medihelp. Overall, the MedElect plan is a great choice for individuals or families looking for comprehensive medical aid coverage and willing to pay a premium for it. However, those on a tight budget may want to consider some of the other more affordable options offered by Medihelp.
You might also consider the following options of MediHelp:
- MediHelp HealthPrint
- MediHelp Medprime
- MediHelp MedPrime Elect
- MediHelp MedPlus
- MediHelp MedElite
- MediHelp MedVital
- MediHelp MedVital Elect
- MediHelp MedSaver
- MediHelp MedMove
- MediHelpMedAdd
- MediHelp MedAdd Elect
MedElect Plan Frequently Asked Questions
What is the MedElect plan offered by Medihelp?
The MedElect plan is a comprehensive medical aid plan offering unlimited hospital cover, generous benefits for chronic medication, and day-to-day medical expenses such as GP consultations, dentistry, and optometry.
What is the cost of the MedElect plan?
The cost of the MedElect plan varies depending on factors such as age, medical history, and the level of coverage required. Therefore, it is best to contact Medihelp directly to obtain a quote.
Does the MedElect plan cover pre-existing medical conditions?
Yes, the MedElect plan does cover pre-existing medical conditions. However, waiting periods may apply.
What are the waiting periods for the MedElect plan?
Waiting periods for the MedElect plan may vary depending on the specific benefit. Generally, waiting periods range from three to 12 months.
Is there a limit on the amount of chronic medication covered by the MedElect plan?
No, there is no limit on the amount of chronic medication covered by the MedElect plan.
Does the MedElect plan cover maternity benefits?
Yes, the MedElect plan does cover maternity benefits, including antenatal care, delivery, and postnatal care.
Are there any network restrictions with the MedElect plan?
No, there are no network restrictions with the MedElect plan. Members are free to choose any healthcare provider, hospital, or pharmacy.
Does the MedElect plan cover dental and optical benefits?
The MedElect plan covers dental and optical benefits, including routine check-ups, fillings, and eyeglasses.
Can I add or remove benefits from the MedElect plan?
No, the benefits of the MedElect plan are fixed and cannot be customized.
How does the MedElect plan compare to other Medihelp plans?
The MedElect plan is one of the premium plans offered by Medihelp. It offers more comprehensive coverage than lower plans such as MedSaver, MedVital, and MedAdd. However, it is more expensive than other plans and may not suit those on a tight budget.
You might also like
Table of Contents
Free Medical Aid Quote
Our Trusted Partners
We work with leading medical aid companies in South Africa.

7 Actionable Ways to save 32% on your MEDICAL AID in 14 days.

- +27 72 7967 530
- [email protected]
- 2nd Floor, West Tower, Nelson Mandela Square, Sandton, 2196, Johannesburg, Gauteng, South Africa
🔎 Report a bug or outdated data to be updated to [email protected]
© Medicalaid.com | All rights Reserved |
Copyright 2024
Top 5 Medical Aids
Top 5 Gap Cover Plans