- Medical Aid
- Currently Trending
The Best Medical Aids
- Compare Plans
- Gap Cover
- Best Gap Covers
- Hospital Plans
- Currently Trending
The Best Hospital Plans
- Medical Insurance
- Pet Insurance
Cape Medical MyHealth 200 Plus Plan
Overall, the Cape Medical MyHealth 200 Plus Plan is a trustworthy and comprehensive medical aid plan that offers 24/7 medical emergency assistance and medical savings to up to 3 Family Members. The Cape Medical MyHealth 200 Plus Plan starts from R9,140 ZAR.
| 🔎 Medical Aid Plan | 🥇 Cape Medical Plan HealthPact Select |
| 👤 Main Member Contribution | R9,140 |
| 👥 Adult Dependent Contribution | R9,140 |
| 🍼 Child Dependent Contribution | R1,476 |
| ➡️ Oncology Cover | 100% CMP tariff |
Cape Medical MyHealth 200 Plus Plan – 7 Key Point Quick Overview
- ☑️ Cape Medical MyHealth 200 Plus Plan Overview
- ☑️ Cape Medical MyHealth 200 Plus Plan Contributions and Medical Savings Account
- ☑️ MyHealth 200 Plus Plan Benefits and Cover Comprehensive Breakdown
- ☑️ MyHealth 200 Plus Plan Exclusions and Waiting Periods
- ☑️ Cape Medical MyHealth 200 Plus Plan vs. Similar Plans from Other Medical Schemes
- ☑️ Our Verdict on The MyHealth 200 Plus Plan
- ☑️ MyHealth 200 Plus Plan Frequently Asked Questions
Cape Medical MyHealth 200 Plus Plan Overview
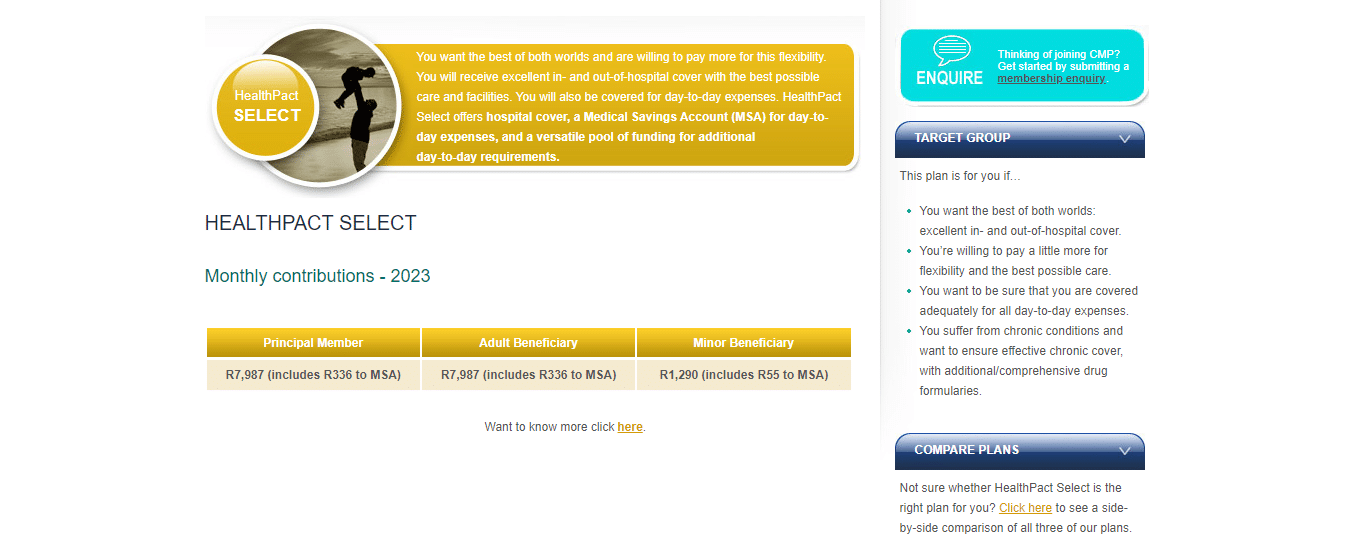
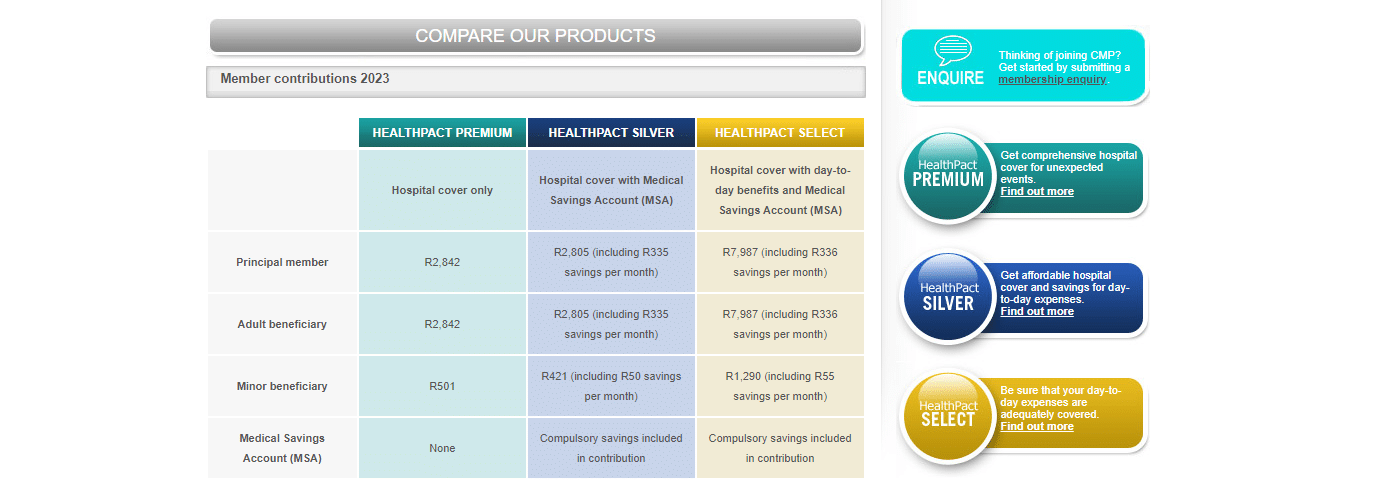
The Cape Medical Plan MyHealth 200 Plus medical aid plan is one of three, starting from R9,140, and includes comprehensive in and out-of-hospital benefits, medical savings, and day-to-day benefits that can help members save on out-of-pocket expenses.
Gap Cover is not available on the Cape Medical Plan MyHealth 200 Plus Plan. However, Cape Medical Plan offers 24/7 medical emergency assistance. According to the Trust Index, Cape Medical Plan has a trust rating of 3.9.
Cape Medical MyHealth 200 Plus Plan Contributions and Medical Savings Account
MyHealth 200 Plus Plan Contributions
| 👤 Main Member | 👥 +1 Adult Dependent | 🍼 +1 Child Dependent |
| R7,987 | R7,987 | R1,290 |
MyHealth 200 Plus Plan Medical Savings Account
| 👤 Main Member | 👥 +1 Adult Dependent | 🍼 +1 Child Dependent |
| R390 per month R4,680 per year | R390 per month R4,680 per year | R64 per month R768 per year |
POLL: 5 Best Hospital Plans under R1500 in South Africa
MyHealth 200 Plus Plan Benefits and Cover Comprehensive Breakdown
MyHealth 200 Plus In-Hospital Benefits
| 🟥 Overall Annual Limit | Unlimited cover in-hospital for authorized admissions. |
| 🟧 Hospital Accommodation Ward Fees Operating Theatre Costs Unattached Theatres Day Hospitals | Covered up to 100% of the CMP tariff or the agreed tariff. Subject to pre-approval. |
| 🟨 Emergency Room treatment (Only) | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. |
| 🟩 Hospitalization for treatment: Mental Illness Alcoholism Drug Addiction | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. Subject to pre-authorization. |
| 🟦 Hospitalisation Alternatives Registered step-down facilities Hospices Registered Nurses Rehabilitation Centres | Covered up to 100% of the CMP tariff for hospices and registered nurses. Limited to 15 days per beneficiary. Subject to pre-approval. |
| 🟪 Emergency Services | Covered up to 100% of the CMP Tariff unless it is a PMB. Subject to pre-authorization. |
| 🟥 Blood Transfusions | Covered up to 100% of the CMP Tariff unless it is a PMB. Subject to pre-authorization. |
| 🟧 Materials and Devices | Covered up to 100% of the cost to a Single Exit Price, Agreed Tariff, or Pre-Authorised Tariff. Subject to pre-approval. |
| 🟨 Medicine | Covered up to 100% of the cost to a Single Exit Price for approved medicines. Subject to pre-authorization. |
| 🟩 Supplementary Services Physiotherapists Occupational Speech Therapists Dieticians | Covered up to 100% of the CMP Tariff. Subject to pre-authorization. |
| 🟦 Consultations, Procedures, and Operations by General Practitioners | Covered up to 200% of the CMP Tariff. Subject to pre-authorization. |
| 🟪 Consultations, Procedures, and Operations by Registered Medical Specialists | Covered up to 200% of the CMP Tariff. Subject to pre-authorization. |
| 🟥 Laparoscopic and Endoscopic Procedures In-Hospital | Covered up to 200% of the CMP Tariff. Subject to pre-authorization. Endoscopic surgeon-guided laparoscopic procedures with a co-payment per scope, per procedure. |
MyHealth 200 Plus Out-of-Hospital Benefits
| 📌 General Practitioner Consultations and Procedures | Covered up to 100% of the CMP tariff. Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. Pre-authorization is required. |
| 📍 Registered Medical Specialist Consultations and Procedures | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. Subject to pre-approval. A written referral is required. |
| 🅰️ Laparoscopic and Endoscopic Procedures | Covered up to 200% of the CMP Tariff. Subject to pre-authorization. Endoscopic surgeon-guided laparoscopic procedures with a co-payment per scope, per procedure. A written referral is required. |
| 🅱️ Supplementary Services Physiotherapists Occupational Speech Therapists Dieticians | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. Subject to pre-approval. |
| 1️⃣ General Dental Practitioner Consultations | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. Subject to pre-approval. |
| 2️⃣ General Dental Practitioner Procedures In-Hospital Procedures | Covered up to 100% of the cost and 120% of the CMP tariff. Covers procedures and operations that require hospitalization unless it is a PMB. Subject to Dental Protocols. |
| 3️⃣ Orthodontic Treatment | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. |
| 4️⃣ Maxillo-Facial Surgeons In-Hospital Procedures | Covered up to 120% of the CMP tariff unless it is a PMB. Subject to pre-authorization. |
| 5️⃣ Maxillo-Facial Surgeons and Orthodontists Dental Implants General Dental Treatment Orthodontic Treatment Orthognathic Procedures Periodontic Treatment and Prosthodontic Treatment | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. |
| ❤️ Maternity Confinement Birth or Delivery | Covered up to 200% of the CMP tariff. Only medically necessary caesareans will be covered unless it is a PMB. Subject to pre-approval. |
| 🧡 Antenatal Consultations and Fetal Scans In and Out-of-Hospital Provided by a Registered Gynaecologist or Radiologist | Covered up to 200% of the CMP tariff. Limited to R3,525 per family annually. Once the limit is reached, claims are paid from the MSA and then the day-to-day pool unless it is a PMB. |
| 💛 Paediatrician Consultations | Covered up to 200% of the CMP tariff. Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. |
| 💚 Paediatrician Procedures and Operations | Covered up to 200% of the CMP tariff. Subject to pre-authorization. |
| 📈 Radiologist Procedures Angiograms CT scans Duplex Doppler Scans International Radiology MRI scans Nuclear Medical Investigations | Covered up to 100% of CMP tariff. Limited to R14,732 per beneficiary per year, with a co-payment of R1,500 per event on all procedures. Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. Pre-approval is required. Written referral required. |
| 🖤 Black and White X-Rays (in-hospital) | Covered up to 100% of the CMP tariff. Subject to pre-authorization. |
| 🤍 Black and White X-Rays (out-of-hospital) | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. |
| ↪️ Mammogram Benefit | Covered up to 100% of CMP tariff Requires a co-payment of R300 per female beneficiary 49 years>. Available once every 2 years. Limited to R1,797. Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. Subject to pre-approval. A registered radiologist must perform it. |
| 🦴 Bone Density Benefit | Covered up to 100% of the CMP tariff per beneficiary once every 5 years for beneficiaries 50 years>. Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. |
| ➡️ Pathology Services In and Out-of-Hospital with Pathcare or Lancet Laboratories | In-and-out pathology is fully covered if you use SANAS-accredited Pathcare or Lancet Laboratories. In-hospital pathology services provided by a provider other than Pathcare or Lancet Laboratories will be covered only during the first 24 hours. If you do not use a Preferred Provider, any out-of-hospital pathology will be paid from available funds in the MSA. |
| 🦾 Prostheses and Implants, excluding: Hearing Devices Dental Implants | Covered up to 100% of the cost if introduced internally as a crucial component in surgery. Subject to CMP prosthetic price list. Limited to R54,000 per beneficiary yearly. Subject to pre-approval. |
| 🦿 External Prostheses and Surgical Appliances Wheelchairs Crutches, etc. | Covered up to 100% of the cost and paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. Subject to pre-authorization. |
| ☑️ Chronic Renal Dialysis | Covered at 100% of the CMP if: PMB level of care criteria is met. Treatment is offered by a Preferred Provider. Subject to pre-approval. |
| 🫀 Organ Transplants | Covered at 100% of the CMP if: PMB level of care criteria is met. Treatment is offered by a Preferred Provider. Subject to pre-approval. |
| ✅ Oncology | Covered at 100% of the CMP according to SA Oncology Consortium Primary Level of Care treatment guidelines if: Formularies and Treatment Protocols of CMP and SA Oncology Consortium tier guidelines are applied according to an agreed treatment plan. Subject to pre-approval. |
| ✔️ Oncology Treatment Anti-emetics Vitamins Cosmetic and Prosthetic Appliances | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. |
| 💊 Chronic Medication | Covered up to 100% of the cost to a Single Exit Price and the Preferred Provider dispensing fee. Subject to the chronic program protocols. |
| 🤧 Acute Medication | 100% of cost to a maximum of SEP, plus the agreed Preferred Provider dispensing fee. Payable from MSA, thereafter from day-to-day pool – except for PMBs. |
| 🤕 Take-home Medication after discharge | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. |
| 😎 Spectacles and Contact Lenses | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. |
| 🔴 Supplementary Services | Paid from the MSA, after that, from the day-to-day pool, unless it is a PMB. |
| 🟠 Mammograms for female beneficiaries | Limited to one per female beneficiary every 2 years. |
| 🟡 Bone Mineral Density Tests | Limited to one per beneficiary every 5 years. |
| 🟢 Pap Smears for female beneficiaries | Female beneficiaries 21 to 65 years, once every 3 years. |
| 🔵 Prostate Test (PSA level) for male beneficiaries | Once yearly for males between 40 and 75 years. |
| 🟣 Antenatal Visits for pregnant beneficiaries | According to CMP guidelines. |
| 🎗️ Voluntary HIV testing and counseling | Once yearly per beneficiary. |
| 💉 Flu Vaccines | Once yearly per beneficiary. |
You might also like the 5 Best Medical Aids under R1500
MyHealth 200 Plus Chronic Conditions and Medication
Access to the chronic medicine benefit is contingent upon CMP’s formularies and protocols. Individuals diagnosed with a chronic condition will likely be required by their physician to adhere to a regimen of regular medication.
While all CMP members are provided coverage for chronic conditions, this coverage is not automatic. Rather, individuals must obtain pre-authorization by enrolling in our Chronic Disease Management program. Upon registration, re-registration will only be necessary if medication changes occur or administrative purposes necessitate it.
The Chronic Disease List (CDL) includes the following covered conditions.
- ✅ Addison’s Disease
- ✅ Anti-coagulating therapy
- ✅ Asthma
- ✅ Bipolar Mood Disorder
- ✅ Bronchiectasis
- ✅ Cardiac failure
- ✅ Cardiomyopathy
- ✅ Chronic Obstructive Pulmonary Disease
- ✅ Chronic Renal Disease
- ✅ Coronary Artery Disease
and many more.
MyHealth 200 Plus Plan Exclusions and Waiting Periods
MyHealth 200 Plus Exclusions
Similar to other medical schemes, there are certain procedures, products, and services that CMP will not cover. As per PMB rules, these exclusions are listed across all products and cannot be paid for from insured benefits. However, they can be paid for using the MSA if funds are available. The following exclusions are applicable:
- ☑️ Procedures to correct eye refraction errors, including blepharoplasties and excimer laser/Lasik
- ☑️ Treatment for sexual dysfunction in males and females
- ☑️ Infertility treatment, except if authorized within PMB level of care criteria
- ☑️ Breast reductions, including scar revision, Botox, breast augmentation, and gynecomastia
- ☑️ MammaPrint genetic testing and any other type of genetic testing
- ☑️ Non-diseased breast reconstruction, nipple reconstruction, and symmetry, unless authorized within PMB level of care criteria
- ☑️ Cosmetic surgery
- ☑️ Long-term nursing care, such as frail care nursing
- ☑️ Non-PMB treatment for alcohol or substance abuse, willful self-injury, or attempted suicide
- ☑️ Non-PMB psychological and psychiatric treatment, including sleep studies
- ☑️ Treatment or surgery for obesity
- ☑️ Educational and group therapy
- ☑️ Protective gear
and many more.
You might like to read more about 10 Easy Ways to Get Cheaper Medical Aid
MyHealth 200 Plus Waiting Periods
New members can be subjected to two types of waiting periods: a general three-month waiting period for all new members and a condition-specific waiting period of up to 12 months. Additionally, a late joiner fee will apply.
Cape Medical MyHealth 200 Plus Plan vs. Similar Plans from other Medical Schemes
| 🔎 Medical Aid Plan | 🥇 Cape Medical Plan HealthPact Select | 🥈 Discovery Health Executive Plan | 🥉 Fedhealth Maxima EXEC |
| 👤 Main Member Contribution | R9,140 | R10,303 | R9,419 |
| 👥 Adult Dependent Contribution | R9,140 | R10,303 | R8,176 |
| 🍼 Child Dependent Contribution | R1,476 | R1,969 | R2,910 |
| ➡️ Oncology Cover | 100% CMP tariff | R500,000 | R624,000 |

Our Verdict on The MyHealth 200 Plus Plan
The MyHealth 200 Plus Saver plan offered by Comprehensive Medical Plan (CMP) is a medical aid plan that provides basic coverage for medical expenses, including in-hospital treatments, chronic medication, and day-to-day medical expenses.
While the plan has some benefits, there are also several disadvantages. One of the main drawbacks of the HealthSaver plan is its much higher premiums compared to other plans that offer more comprehensive coverage.
You might also consider the following options Cape Medical has to offer:
- 👉 Cape Medical Plan Review
- 👉 Cape Medical Plan MyHealth 200
- 👉 Cape Medical Plan MyHealth 100 Saver
- 👉 Cape Medical Plan Late Joiner Fee
MyHealth 200 Plus Plan Frequently Asked Questions
What is Cape Medical Plan?
Cape Medical Plan is a South African healthcare provider offering various medical aid plans to individuals and families.
What is the MyHealth 200 Plus plan?
The MyHealth 200 Plus plan is a medical aid plan offered by Cape Medical Plan that provides comprehensive cover for medical expenses, including hospitalization, chronic medication, and day-to-day medical expenses.
What is a medical aid plan?
A medical aid plan is a type of health insurance covering medical expenses, such as hospitalization, consultations with healthcare professionals, and prescribed medication.
What is health insurance?
Health insurance is a type of insurance that provides coverage for medical expenses.
What is hospitalization coverage?
Hospitalization cover is a medical aid benefit covering the cost of medical treatment received in a hospital.
What is chronic medication?
Chronic medication is prescribed to manage a chronic condition, such as diabetes or hypertension.
What are day-to-day medical expenses?
Day-to-day medical expenses are medical expenses that are incurred outside of a hospital setting, such as consultations with healthcare professionals, laboratory tests, and prescribed medication.
How can I contact Cape Medical Plan?
You can contact Cape Medical Plan by calling their customer service line at 0860 102 493 or by visiting their website and filling out a contact form.
What are Cape Medical Plan’s operating hours?
Cape Medical Plan’s customer service line operates from Monday to Friday, 8 am to 5 pm.
Where are Cape Medical Plan’s offices located?
Cape Medical Plan’s offices are located in Cape Town, South Africa.
Where can I find reviews of the Cape Medical Plan?
You can find reviews of Cape Medical Plan on their website and third-party review websites.
What do Cape Medical Plan reviews say about the company?
Cape Medical Plan reviews vary, but generally, customers report positive experiences with the company’s customer service and comprehensive medical aid plans.
What is Cape Medical Plan authorization?
Cape Medical Plan authorization is obtaining approval from the company before receiving certain medical treatments or procedures.
How do I obtain authorization from Cape Medical Plan?
You can obtain authorization from Cape Medical Plan by contacting their customer service line or submitting an authorization request through their online portal.
How do I submit a claim to Cape Medical Plan?
You can submit a claim to Cape Medical Plan by completing a claims form, which is available on their website, and submitting it along with any relevant receipts or documentation.
How long does it take for Cape Medical Plan to process a claim?
The time it takes for Cape Medical Plan to process a claim varies. However, generally, claims are processed within 5 to 7 business days.
How will I be reimbursed for my claim?
Cape Medical Plan typically reimburses claims directly to the member’s bank account.
What types of expenses are covered by Cape Medical Plan?
Cape Medical Plan covers a range of medical expenses, including hospitalization, chronic medication, and day-to-day medical expenses.
What is the out-of-pocket expense for Cape Medical Plan?
The out-of-pocket expense for Cape Medical Plan varies depending on the individual or family’s medical aid plan and their specific healthcare needs. Therefore, contacting Cape Medical Plan directly is recommended for more information.
What is the reimbursement rate for Cape Medical Plan?
The reimbursement rate for Cape Medical Plan varies depending on the medical expense and the individual or family’s medical aid plan. Therefore, contacting Cape Medical Plan directly is recommended for more information.
How can I check the status of my claim with Cape Medical Plan?
You can check the status of your claim with Cape Medical Plan by logging into their online portal or by contacting their customer service line.
What should I do if Cape Medical Plan rejects my claim?
If Cape Medical Plan rejects your claim, you can contact their customer service line to discuss the reason for the rejection and to see if there are any options for appeal or reconsideration.
You might also like
Table of Contents
Free Medical Aid Quote
Our Trusted Partners
We work with leading medical aid companies in South Africa.

7 Actionable Ways to save 32% on your MEDICAL AID in 14 days.

- +27 72 7967 530
- [email protected]
- 2nd Floor, West Tower, Nelson Mandela Square, Sandton, 2196, Johannesburg, Gauteng, South Africa
🔎 Report a bug or outdated data to be updated to [email protected]
© Medicalaid.com | All rights Reserved |
Copyright 2024
Top 5 Medical Aids
Top 5 Gap Cover Plans
































