- Medical Aid
- Currently Trending
The Best Medical Aids
- Compare Plans
- Gap Cover
- Best Gap Covers
- Hospital Plans
- Currently Trending
The Best Hospital Plans
- Medical Insurance
- Pet Insurance
Medshield MediCurve Medical Aid Plan
Overall, the Medshield MediCurve Medical Aid Plan is a trustworthy and comprehensive medical aid plan that offers 24/7 medical emergency assistance and major medical benefits to up to 3 Family Members. The Medshield MediCurve Medical Aid Plan starts from R1,584 ZAR.
| 👤 Main Member Contribution | R1,584 |
| 👥 Adult Dependent Contribution | R1,584 |
| 🍼 Child Dependent Contribution | R1,584 |
| 🔁 Gap Cover | None |
| ☑️ Hospital Cover | Unlimited |
| ➡️ Oncology Cover | Unlimited, subject to PMBs |
| 💶 rescribed Minimum Benefits | ✅ Yes |
| 📉 Screening and Prevention | ✅ Yes |
| 📌 Medical Savings Account | None |
| 📍 Maternity Benefits | ✅ Yes |
Medshield MediCurve Plan – 14 Key Point Quick Overview
- ✅ Medshield MediCurve Plan Overview
- ✅ Medshield MediCurve Plan Contributions
- ✅ Medshield MediCurve Plan Benefits and Cover Comprehensive Breakdown
- ✅ Medshield MOM Program and Benefits
- ✅ MediCurve Out-of-Hospital Benefits
- ✅ MediCurve SmartCare Services and Benefits
- ✅ MediCurve Wellness Benefits
- ✅ MediCurve Ambulance and Emergency Services
- ✅ MediCurve Prescribed Minimum Benefits
- ✅ MediCurve COVID-19 Benefits and Access to Care
- ✅ MediCurve Plan Exclusions and Waiting Periods
- ✅ Medshield MediCurve Plan vs. Similar Plans from Other Medical Schemes
- ✅ Our Verdict on The MediCurve Plan
- ✅ MediCurve Plan Frequently Asked Questions
Medshield MediCurve Plan Overview
The Medshield MediCurve medical aid plan is one of 11, starting from R1,584, and includes family practitioners, wellness, dentistry, emergency services, major medical benefits in-hospital, and more. Gap Cover is not available on the Medshield MediCurve Plan. However, Medshield offers 24/7 medical emergency assistance. According to the Trust Index, Medshield has a trust rating of 4.1.
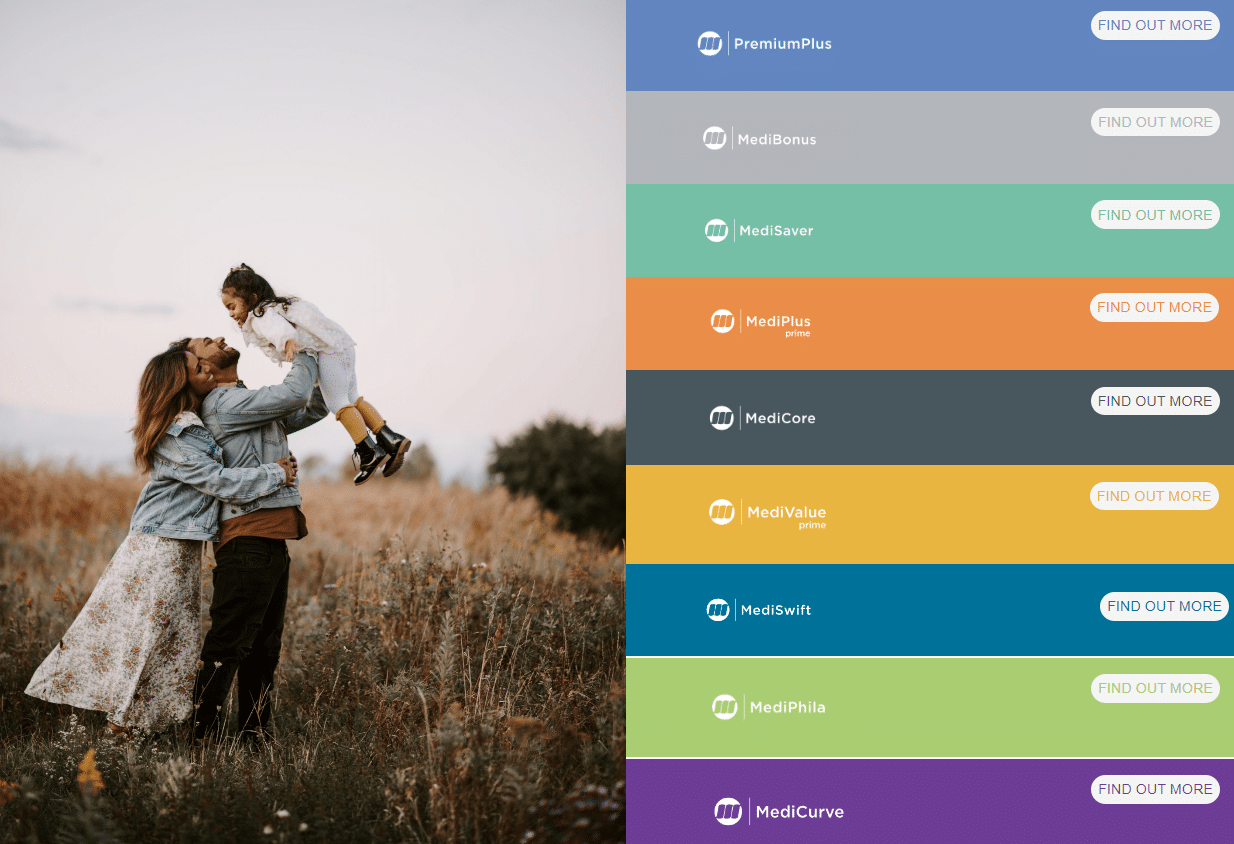
MedShield has the following medical aid plans to offer:
- MedShield MediCurve
- MedShield PremiumPlus
- MedShield MediValue Prime
- MedShield Value Compact
- MedShield MediSwift
- MedShield MediSaver
- MedShield MediPlus Prime
- MedShield MediPlus Compact
- MedShield MediPhila
- MedShield MediCore
- MedShield MediBonus
Medshield MediCurve Plan Contributions
| 👤 Main Member | 👥 +1 Adult Dependent | 🍼 +1 Child Dependent |
| R1,584 | R1,584 | R1,584 |
Discover the 5 Best Medical Aids under R200
Medshield MediCurve Plan Benefits and Cover Comprehensive Breakdown
MediCurve Hospital-At-Home
- Medshield offers a Hospital-at-Home service delivered by Quro Medical.
- The Hospital-at-Home service offers an alternative to hospitals as the center of patient care and management.
- Hospital-at-Home provides active treatment at home instead of a general hospital ward for a specified period without compromising the quality of care.
- Patients more vulnerable to hospital-acquired infections and developing new health complications may benefit from care at home.
- Patients who usually need admission to a general hospital ward are eligible for Hospital-at-Home.
- Quro Medical works with each patient and their treating doctor to develop a personalized treatment plan that can be delivered at home.
- Treatment plans are amended accordingly if a patient’s medical needs change during treatment.
- The clinical team at Quro Medical arranges routine home visits customized to the individual’s specific needs that may occur daily or more frequently to provide the necessary treatment and care.
- Other channels allow patients to access advice and support outside of home visits.
MediCurve Major Medical Benefits In-Hospital
| 🟥 Overall Annual Limit | There is no overall annual limit on hospitalization. |
| 🟧 Hospitalization | Subject to pre-approval. Specialist services are covered by treating/attending doctors. PMBs Unlimited cover. Non-PMBs 25% co-payment when using a non-MediCurve Network Hospital. |
| 🟨 Medicine upon discharge | Limited to R455 per admission. Per the Maximum Generic Pricing of Medicine Price List and Medshield Formulary. |
| 🟩 Hospitalization Alternatives Physical Rehabilitation Sub-Acute Facilities Nursing Services Hospice Terminal Care | Clinical Protocols will apply. Limited to R30,600 per family per year. Subject to PMB and PMB level of care. 25% co-payment for using a non-MediCurve Network Hospital. Terminal care is limited to R12,660 per family per year and is subject to the overall limit on hospitalization alternatives. |
| 🟦 Blood, Blood Equivalents, and Blood Products | Unlimited cover. |
| 🟪 Medical Practitioner Consultations and Visits during Hospital Admission | Unlimited cover. Subject to Pathology Formulary List. |
| 🟥 Organ, Tissue, and Haemopoietic Stem Cell (Bone Marrow) Transplants | Unlimited cover. Subject to PMB and PMB level of care. 25% co-payment for using a non-MediCurve Network Hospital. Limited to harvests in South Africa. Solid organ transplant donor work-up fees. No international donor search benefits. Bone marrow transplantation is confined to allogenic and autologous grafts from the South African Bone Marrow Registry. |
| 🟧 Pathology and Medical Technology | Unlimited cover. |
| 🟨 Physiotherapy | Limited to R2,955 per beneficiary yearly and no benefit after that unless pre-authorized. |
| 🟩 Internal Prostheses and Devices | Subject to pre-authorization by the relevant Managed Healthcare Program. Unlimited with PMB and PMB treatment. Members must use Rand One as the DSP. Hips and knees sub-limit R35,510 per beneficiary (subject to PMB and PMB level of care). Non-MediCurve Network Hospital attracts a co-payment of 25%. |
| 🟦 External Prostheses | Unlimited but subject to PMB and PMB level of care. |
| 🟪 Basic Radiology | Unlimited cover. |
| 🟥 Specialized Radiology | Limited to R5,500 per family per year both in and out of the hospital. Clinical Protocols apply |
| 🟧 CT Scans, MUGA Scans, MRI Scans, Radio Isotope Studies | Subject to the Specialized Radiology Limit |
| 🟨 CT Colonography (Virtual colonoscopy) | There is no co-payment. |
| 🟩 Interventional Radiology Replacing Surgical Procedures | Unlimited cover. |
| 🟦 Chronic Renal Dialysis Material Medication Related Radiology and Pathology | Unlimited if PMB and PMB level of care are met. A non-DSP will incur a 35% upfront co-payment. Use of a DSP with Rand one for PMB admittance. |
| 🟪 Non-Surgical Procedures and Tests | Unlimited cover. Medshield Specialist Network might apply. |
| 🟥 Mental Health | Subject to pre-authorization by the relevant Managed Healthcare Program. The Medshield Specialist Network may be utilized. Limited to a maximum of three days if admitted by a family physician. Unlimited if PMB and PMB level of care are met. A non-DSP will incur a 25% upfront co-payment. Use of a DSP with Rand one for PMB admittance. |
| 🟧 Rehabilitation for Substance Abuse | Subject to PMB and PMB level of care. |
| 🟨 Consultations and Visits, Procedures, Assessments, Therapy, Treatment, or Counselling | Subject to PMB and PMB level of care. |
| 🟩 HIV and Aids | According to the Managed Healthcare Protocols. Pre-authorization and Managed Healthcare Program registration are required. |
| 🟦 Anti-retroviral and related medicines | Voluntary out-of-formulary or PMB medication from a non-DSP supplier requires a 35% upfront co-payment. Courier DSP – Rand one. |
| 🟪 HIV/AIDS-related Pathology and Consultations | Voluntary out-of-formulary or PMB medication from a non-DSP supplier requires a 35% upfront co-payment. Courier DSP – Rand one. |
| 🟥 National HIV Counselling and Testing (HCT) | Voluntary out-of-formulary or PMB medication from a non-DSP supplier requires a 35% upfront co-payment. Courier DSP – Rand one. |
| 🟧 Infertility Interventions and Investigations | Clinical Protocols apply. Limited to interventions and investigations only. Pre-authorization and Managed Healthcare Program registration are required. |
You might like to read more about 5 Best Hospital Plans under R2000 in South Africa
MediCurve Dentistry Benefits
| 🅰️ Basic Dentistry | According to the Dental Managed Healthcare Programme, Protocols, and the Medshield Dental Network. Beneficiaries pay R150 upfront for one dental exam every six months. |
| 🅱️ Impacted Teeth, Wisdom Teeth, and Apicectomy | Subject to the overall annual limit. Day Clinic wisdom teeth extraction requires an R1,800 upfront co-payment. In-hospital pre-authorization requires R4,000 upfront co-payment. However, in Practitioners’ offices, conscious sedation does not require co-payment. Only hospitalization, general anesthetics, or conscious sedation for bone impactions. Practitioners only cover out-of-hospital apicectomy of permanent teeth. Pre-authorization and Hospital Managed Healthcare Programs. Dental Managed Healthcare Programs, Protocols, and Medshield Dental Network. General anesthesia and conscious sedation pre-authorization, in- and out-of-hospital. Apicectomy, impacted tooth removal, and wisdom tooth removal under local anesthesia do not require authorization. |
| 📌 Maxillo-Facial Surgery | All services are subject to pre-authorization by the relevant Managed Healthcare Program. Under the Hospitalization Limit, R5,500 per household per year. In-hospital pre-authorization requires R4,000 upfront co-payment. Non-elective surgery only. Subject to Dental Managed Healthcare Programs and Protocols. MediCurve Hospital Network services are required. Use of the Medshield Specialist Network might apply. |
MediCurve Oncology Benefits
| 🔴 Oncology Limit | Unlimited cover. Subject to PMB and PMB level of care. |
| 🟠 Active Treatment (Includes Stoma Therapy, Incontinence Therapy, and Brachytherapy) | Subject to the Oncology Limit. ICON Standard Protocols apply. |
| 🟡 Oncology Medicine | Subject to the Oncology Limit. ICON Standard Protocols apply. |
| 🟢 Radiology and Pathology | Subject to the Oncology Limit. |
| 🔵 PET and PET-CT | Limited to 1 Scan per family per annum. Subject to the Oncology Limit. |
| 🟣 Integrated Continuous Cancer Care | Six visits per family per annum. Subject to the Oncology Limit |
| 🔴 Specialized Drugs for Oncology, Non-Oncology, and Biological Drugs | Subject to the Oncology Limit. |
| 🟠 Vitreoretinal Benefit | Subject to PMB and PMB level of care. |
| 🟡 Breast Reconstruction | R94,105 per family yearly. Breast Reconstruction is exempt from prosthesis co-payments and limits. The applicable Managed Healthcare Program must pre-authorize DSP or Network Provider services. Medshield Specialist Network may apply. Post-mastectomy protocols apply. |
MediCurve Chronic Medicine Benefits
- Using a MediCurve Chronic Network Pharmacy from Rand one
- Exclusive to PMB exclusively.
- Medicines will be approved according to the Medshield Formulary, with coverage from Rand One.
- Use of a non-MediCurve Chronic Network Pharmacy will incur an upfront co-payment of 35%.
- Supply of Medication (One month in advance)
- Exclusive to PMB exclusively.
- Medicines will be approved according to the Medshield Formulary, with coverage from Rand One.
- Use of a non-MediCurve Chronic Network Pharmacy will incur an upfront co-payment of 35%.
MediCurve Chronic Disease List
- Addison’s disease
- Asthma
- Bi-Polar Mood Disorder
- Bronchiectasis
- Cardiac failure
- Cardiomyopathy
- Chronic renal disease
- Chronic obstructive pulmonary disease
- Coronary artery disease
- Crohn’s disease
and many more.
MediCurve Maternity Benefits
- There will be benefits during pregnancy, after birth, and following delivery. However, pre-authorization with the applicable Managed Healthcare Program is required before hospital admission.
- Unless otherwise specified, benefits are allocated for each pregnancy subject to the Total Yearly Limit.
- A complimentary baby bag from Medshield can be obtained during the third trimester.
| 👶 Antenatal Consultations | 6 Consultations per pregnancy. It might be subject to the use of the Medshield Specialist Network. |
| 🍼 Antenatal Classes and Postnatal Midwife Consults | 4 Visits per event. |
| 💗 Scans | Two 2D scans per pregnancy. |
| Tests | One Amniocentesis test per pregnancy. |
| ➡️ Confinement and postnatal Consultations | Use of a non-DSP requires an upfront co-payment of 25%. Members must use a DSP from Rand One. Subject to prior authorization by the applicable Managed Healthcare Program. MediCurve Network services must be purchased. |
| ↪️ Confinement In-Hospital | Unlimited / Clinical Protocols apply. |
| ☑️ Confinement in a registered birthing unit or Out-of-Hospital Confinement in a registered birthing unit or Out-of-Hospital | Unlimited / Clinical Protocols apply. |
| 🅰️ Delivery by a registered Midwife or a Practitioner | Unlimited / Clinical Protocols apply. |
| 🅱️ Hire of a water bath and oxygen cylinder | Unlimited / Clinical Protocols apply. |
READ more about 5 Best Medical Aids in South Africa Cover IVF
Medshield MOM Program and Benefits
To support women on their journey to motherhood, Medshield MOM has launched a dedicated website that provides information and resources for all stages of pregnancy, birth, and postpartum. This website is an easily accessible hub of valuable health, fitness, nutrition, motherhood, babies, toddlers, and more content specifically tailored to the pre-and post-partum phases. As a Medshield member, you can take advantage of the pregnancy-related benefits. The Medshield MOM website will ensure you are fully informed of your options. Some of the features and advantages include, but are not limited to, the following:
- A guide for your journey from start to finish.
- Convenient, dependable, and easily accessible pregnancy resources.
- A toddler benefit that includes information on child immunization, child nutrition, a nurse helpline available 24/7, and digital/online kid yoga.
- Advice formulated by professionals.
- Reminders through email to arrange doctor’s appointments and request hospital pre-authorizations, etc.
- Emails containing updates on your unborn child’s growth and development.
- Mothers can register and enter the specific week of their pregnancy journey. Then, they will begin getting content based on that time and continuing ahead.
The Medshield MOM bags are made locally utilizing recyclable, eco-friendly materials. These distinctive bags are filled with wonderful Bennetts products for your child.
MediCurve Out-of-Hospital Benefits
| 🅰️ Family Practitioner (FP) Consultations and Visits FP consults and visits are available in person, over the phone, and remotely. Each beneficiary is required to select ONE Family Practitioner from the MediCurve Family Practitioner (FP) Network. From Rand one, the MediCurve FP Network is applicable. | Unlimited cover. There is an R100 upfront co-payment for every visit. |
| 🅱️ Registered Chronic Beneficiaries extended FP consults and visits (when you have not consulted a nominated FP) | The Chronic Disease List applies to this benefit. Two for each recipient from the Yearly limit. Subject to enrollment in the applicable Disease Management Program. Subject to using the MediCurve Family Practitioner Network. |
| 🟥 Non-Nominated FP Consultations and Visits | Two visits per household per year. An R100 upfront co-payment is required, followed by an additional 40% upfront co-payment. |
| 💊 Acute Medicine | The designated FP must prescribe it. Medshield formularies must be followed. Dependent on the utilization of the Medshield Pharmacy Network. Limited to R580 per household annually. There is an R10 co-payment per medication line item. |
| 👩⚕️ Pharmacy Advised Therapy (PAT) | Restricted to Schedules 0, 1, and 2 medications recommended and supplied by pharmacists. Members must use the Medshield Pharmacy Network. R365 per family. Limited to R105 per script, One script per beneficiary per day. |
| 🤓 Optometry | Subjected to applicable Optometric Managed Healthcare Program and Procedures Limited to R895 per beneficiary every 24 months, defined by the dating cycle of optical service. |
| 👁️ Optometric Refraction Eye Tests | One test per beneficiary per 24-month optical cycle. There is an R100 upfront co-payment. |
| 👁️🗨️ Spectacles or Contact Lenses | There is an R100 upfront co-payment. Subject to Optical Limit. |
| 🟨 Reading Glasses | There is a limit of R190 per beneficiary. Subject to Optical Limit. |
| 📉 Pathology and Medical Technology | Subject to PMB. Subject to the relevant Pathology Managed Healthcare Program and Protocols. |
| 📈 Covid-19 PCR/Antigen Test | The 1st test is included in the overall annual limit, and subsequent tests provide no benefit unless the result is positive and subject to PMB. |
| 📊 Specialized Radiology | Limited to R5,500 In- and Out-of-Hospital, per family yearly. Subject to pre-authorization by the relevant Managed Healthcare Program |
| 🧪 Non-Surgical Procedures and Tests | Members must use the Medshield Specialist Network. |
| 📌 Routine diagnostic Endoscopic Procedures performed in the Practitioner’s rooms | Subject to Overall Yearly Limit if performed in the Practitioner’s office. There is a co-payment of R2,000 if the procedure is pre-authorized and performed in-hospital. In-Hospital co-payments are not applicable for children under 8 years old. |
| 📍 Intrauterine Devices and Alternatives | Covers consultation, pelvic ultrasound, sterile tray, device, and insertion, if performed the same day. Subject to the applicable clinical protocols. The Medshield Specialist Network must be utilized. It should be performed at the practitioner’s office. Only covered if no hormonal contraceptives are taken, but only upon application Limited to 1 per female recipient. Subject to the Yearly Maximum Limit. Included are all IUD brands up to the cost of the Mirena device. One Mirena/Kyleena device per female patient every five years. Implanon – one per female recipient every three years. One Nova T/Copper device per female patient every two years. |
Discover: Hospital Plans
MediCurve SmartCare Services and Benefits
SmartCare gives access to Videomed and telephone video consultations through a select group of healthcare professionals. SmartCare is a developing healthcare benefit aiming to provide members with convenient care access.
SmartCare services include the following:
- Acute Consultations – Infections of the chest and upper respiratory tract, urinary tract, eyes, ears, etc.
- Chronic Consultations – Medication and refills for hypertension, diabetes, excessive cholesterol, etc. Then, members are advised to utilize the Medshield Chronic Medication Courier Service DSP to have their chronic medication delivered directly to their home or place of business.
| 🟩 Pharmacy/clinic private nurse practitioner consultations | Unlimited cover. |
| 🟦 Nurse-led Videomed family practitioner (FP) consultations | Unlimited cover. |
| 🟪 WhatsApp doc advice line | Unlimited cover. |
MediCurve Wellness Benefits
Medshield’s Wellness Benefit program empowers members to proactively manage their health by undergoing preventative tests and procedures. The company strongly advises its members to schedule the necessary tests at least once per year. To access the Wellness Benefits, Medshield members must use pharmacies included in their benefit options Pharmacy Network. Members must note that benefits are subject to the Overall Annual Limit. Once that limit has been reached, the benefits will be subject to the Day-to-Day limit. However, consultations for certain services are excluded from these limits.
| ❤️ Birth Control (Contraceptive Medicine) | Limited to a maximum of 13 prescriptions per year per female recipient between the ages of 14 and 55, with an R165 limit per prescription. Subject to Acute Medical Benefit Limit. Only relevant in the absence of intrauterine devices and alternatives. |
| 🧡 COVID-19 Vaccines | Subject to the Overall Annual Limit. Protocols apply. |
| 💛 Flu Vaccines | One per beneficiary aged 18 or older is included in the Yearly limit. There is no benefit after that. |
| 💚 Pap Smear | One per female beneficiary. |
| 💙 Health Risk Assessment on the SmartCare Network Cholesterol Blood Glucose Blood Pressure Body Mass Index (BMI) | One per beneficiary 18> |
| 💜 National HIV Counselling Testing (HCT) | One test per beneficiary. |

MediCurve Ambulance and Emergency Services
A 24-hour Hotline will be available to members and their registered dependents. In addition, members can dial 086 100 6337 to reach the Ambulance and Emergency Services, provider.
Medshield Emergency Medical Services:
- Subject to pre-approval by the supplier of Ambulance and Emergency Services.
- Air Evacuation necessitates scheme approval.
- Applying Clinical Procedures.
MediCurve Prescribed Minimum Benefits
Medshield members are entitled to coverage for Prescribed Minimum Benefits (PMBs), regardless of their chosen benefit option. Medshield assumes the cost of PMB treatments if they are provided by one of Medshield’s Designated Service Providers (DSPs) in compliance with the Scheme Rules. The Medical Schemes Act 131 of 1998 mandates that all medical plans must cover the costs associated with the following:
- Any potentially fatal medical emergency
- A set of 26 Chronic Disease List (CDL) diseases that are well-defined
- 271 DTP diagnoses.
How Medshield Covers PMBs under MediCurve
| 🏥 In-Hospital Admissions for treating PMBs | If you are diagnosed with a PMB disease requiring hospitalization, you must comply with the Medshield hospital authorization process. It would help if you utilized a hospital that is a part of the Hospital Network for your selected insurance package, as all stay and treatment fees have negotiated prices. Specialist services obtained during hospitalization are reimbursed at the Scheme rate. If the Scheme rate does not cover the entire claim amount, you must apply to the Scheme and request that the Specialist’s rate be paid at cost instead of the Scheme rate. |
| 🚑 Out-of-Hospital treatment and managing PMBs | Members diagnosed with any of the 26 CDL conditions covered by Medshield and MediCurve must apply to Mediscor for approval. The member automatically receives a Care Plan (treatment plan) notification from the Scheme after the healthcare provider claims with the ICD-code as authorized. The Care Plan details and approves benefits like radiography, pathology, and doctors’ visits. The member and their treating provider must fill out a PMB Application form to seek clearance for further treatment after the Care Plan has been used. If approved, a revised Care Plan will include the additional treatment. |
| 🅰️ MediCurve Option Payment for PMB conditions | Risk pays directly for the expenses of treatment outlined in Care Plans (OAL). Members requiring extra therapy must submit a PMB application form. |
| 🅱️ 271 DTP Conditions | Members with DTP must complete a PMB application form with their doctor. If they do not complete a PMB Application form, the Day-to-Day Savings will pay for treatment. The Care Plan (treatment plan) will list the covered treatments for the condition after clinical assessment and approval. |
| 📍 COVID-19 as a PMB | Respiratory DTP PMB includes Covid-19. After seeing a doctor, members might need a COVID-19 PCR or SARS-CoV-2 Antigen test. According to the Plan Regulations, this benefit requires a doctor or nurse referral and payment. MediCurve covers either a PCR or an antigen test, but not both. |
POLL: 5 Best Medical Aid for Unemployed in South Africa
MediCurve COVID-19 Benefits and Access to Care
The COVID-19 PCR Test or Antigen Tests have the following features and conditions:
- The First COVID PCR or antigen test is covered in the Overall Annual Limit (OAL).
- Depending on the option, the Second and subsequent tests are covered by day-to-day limits or a medical savings plan. If these benefits are not available, members must pay for the tests.
- The 2nd and subsequent positive PCR or Antigen tests are covered first from Day-to-Day benefit or Savings, then from OAL if PMB applies.
- The pathology test will be reimbursed as a PMB by Risk after emailing the positive results to Medshield. Risk
- Benefits require a PMB Application form, and Clinical Protocols apply.
- Travel and non-symptomatic COVID-19 tests are excluded from this benefit.
- Scheme risk gives members the Day-to-Day restriction. Therefore, PMB COVID-19 treatment will pay from a Day-to-Day benefit until it is gone and then from Risk (OAL).
MediCurve Plan Exclusions and Waiting Periods
MediCurve Exclusions
MediCurve does not cover the following:
- Alternative Healthcare Practitioners
- Herbalists
- Therapeutic Massage Therapy (Masseurs)
- Aromatherapy
- Ayurvedics
- Iridology
- Reflexology
- Selected Appliances, External Accessories, and Orthotics
- Blood, Blood Equivalents, and Blood Products
- Hemopure (bovine blood), unless there is an acute shortage of human blood and blood products for acutely anemic patients
- Dentistry Exclusions as determined by the Schemes Dental Management Program
- Preventative Care
- Oral hygiene instruction
- Oral hygiene evaluation
- Fillings/Restorations Fillings to restore teeth damaged due to toothbrush abrasion, attrition, erosion, and fluorosis
- Resin bonding for restorations is charged as a separate procedure from the restoration.
Note: A full list will be provided.
MediCurve Waiting Periods
Often, there is a waiting period for pre-existing conditions. This is to prevent new members from abusing medical insurance for a short period to finance pricey procedures and then canceling their membership shortly after. According to the Medical Schemes Act No. 131 of 1998, the following waiting periods may apply:
- A 3 (three) month general waiting time for all benefits.
- A maximum 12 (twelve) month exclusion for a previous ailment.
A late joiner contribution penalty.
Medshield MediCurve Plan vs. Similar Plans from Other Medical Schemes
| 🔎 Medical Aid Plan | 🥇 Medshield MediCurve | 🥈 Bestmed Beat 1 | 🥉 Medihelp MedMove! |
| 👤 Main Member Contribution | R1,584 | R2,082 | R |
| 👥 Adult Dependent Contribution | R1,584 | R1,616 | R |
| 🍼 Child Dependent Contribution | R1,584 | R875 | R |
| 📊 Annual Limit | Unlimited Hospital Cover | Several limits and sub-limits | Unlimited Hospital Cover |
| 💙 Hospital Cover | Unlimited | Subject to scheme rules | Unlimited |
Our Verdict on The MediCurve Plan
Overall, Medshield’s MediCurve plan is a comprehensive medical aid offering that gives members access to a range of benefits, including in-hospital and out-of-hospital care. The plan features an extensive network of healthcare providers, ensuring members have access to quality healthcare services across South Africa. Furthermore, even as an entry-level plan, MediCurve offers comprehensive cover for maternity, chronic conditions, oncology, dentistry, optometry, internal and external prostheses, and more. However, there is limited out-of-hospital coverage, and many co-payments apply, especially when members do not use a provider or facility within the MediCurve network, which could limit the treatment options.
You might also like the following plans MedShield has to offer:
- ✅ MedShield PremiumPlus
- ✅ MedShield MediValue Prime
- ✅ MedShield Value Compact
- ✅ MedShield MediSwift
- ✅ MedShield MediSaver
- ✅ MedShield MediPlus Prime
- ✅ MedShield MediPlus Compact
- ✅ MedShield MediPhila
- ✅ MedShield MediCore
- ✅ MedShield MediBonus
MediCurve Plan Frequently Asked Questions
What is MediCurve?
MediCurve is a comprehensive medical aid plan offered by Medshield that covers both in-hospital and out-of-hospital medical expenses.
What are the benefits of MediCurve?
MediCurve provides members access to a range of benefits, including chronic medication coverage, hospital coverage, and flexible savings accounts.
How much does the MediCurve plan cost?
MediCurve costs R1,584 for the main member and per adult and child dependent. Members should note that co-payments are paid out-of-pocket.
Does MediCurve cover chronic medication?
Yes, MediCurve covers the chronic medication, subject to certain conditions and limits.
Does MediCurve provide hospital cover?
Yes, MediCurve includes hospital cover, and members can access a network of healthcare providers across South Africa.
Can I choose my healthcare provider with MediCurve?
Yes, MediCurve members have access to a network of healthcare providers across South Africa, and they can choose their preferred provider.
Does MediCurve offer a savings account?
No, MediCurve does not offer a savings account. Instead, the plan covers treatments, medications, services, and procedures from an overall limit and daily benefit.
How do I enroll in MediCurve?
To enroll in MediCurve, visit the Medshield website or contact their customer service team for assistance. You can complete the application form, provide the supporting documents, and await approval.
Can I change my benefit option under the MediCurve plan?
Yes, members can change their benefit option under the MediCurve plan during the annual open enrollment period. However, changes outside this period may be subject to certain conditions and limitations.
You might also like
Table of Contents
Free Medical Aid Quote
Our Trusted Partners
We work with leading medical aid companies in South Africa.

7 Actionable Ways to save 32% on your MEDICAL AID in 14 days.

- +27 72 7967 530
- [email protected]
- 2nd Floor, West Tower, Nelson Mandela Square, Sandton, 2196, Johannesburg, Gauteng, South Africa
🔎 Report a bug or outdated data to be updated to [email protected]
© Medicalaid.com | All rights Reserved |
Copyright 2024
Top 5 Medical Aids
Top 5 Gap Cover Plans