- Medical Aid
- Currently Trending
The Best Medical Aids
- Compare Plans
- Gap Cover
- Best Gap Covers
- Hospital Plans
- Currently Trending
The Best Hospital Plans
- Medical Insurance
- Pet Insurance
Medshield MediBonus Medical Aid Plan
Overall, the Medshield MediBonus Medical Aid Plan is a trustworthy and comprehensive medical aid plan that offers 24/7 medical emergency assistance and in-hospital procedures to up to 3 Family Members. The Medihelp MedAdd Medical Aid Plan starts from R7,587 ZAR.
| 👤 Main Member Contribution | R7,587 |
| 👥 Adult Dependent Contribution | R5,328 |
| 🍼 Child Dependent Contribution | R1,578 |
| 🌎 International Cover | Only Organ Transplants |
| 🔁 Gap Cover | None |
| ⚕️ Hospital Cover | Unlimited |
| 🏠 Home Care | ☑️ Yes |
| 📌 Medical Savings Account | None |
| 💶 Prescribed Minimum Benefits | ☑️ Yes |
| 📍 Oncology Cover | R552,925 |

Medshield MediBonus – 14 Key Point Quick Overview
- ☑️ Medshield MediBonus Overview
- ☑️ Medshield MediBonus Plan Contributions
- ☑️ Medshield MediBonus Plan Benefits and Cover Comprehensive Breakdown
- ☑️ MediBonus Chronic Disease List
- ☑️ MediBonus Dentistry Benefits
- ☑️ MediBonus Maternity Benefits
- ☑️ Medshield MOM Program and Benefits
- ☑️ MediBonus SmartCare Services and Benefits
- ☑️ MediBonus Prescribed Minimum Benefits
- ☑️ MediBonus COVID-19 Benefits and Access to Care
- ☑️ MediBonus Plan Exclusions and Waiting Periods
- ☑️ Medshield MediBonus Plan vs. Similar Plans from other Medical Schemes
- ☑️ Our Verdict on The MediBonus Plan
- ☑️ MediBonus Plan Frequently Asked Questions
Medshield MediBonus Overview
The Medshield MediBonus medical aid plan is one of 11, starting from R7,587 and includes In-Hospital procedures covered up to 200%, generous day-to-day limits, quick and streamlined claims procedures, hospital-at-home benefits, and more. Gap Cover is not available on the Medshield MediBonus Plan. However, Medshield offers 24/7 medical emergency assistance. According to the Trust Index, Medshield has a trust rating of 4.1.
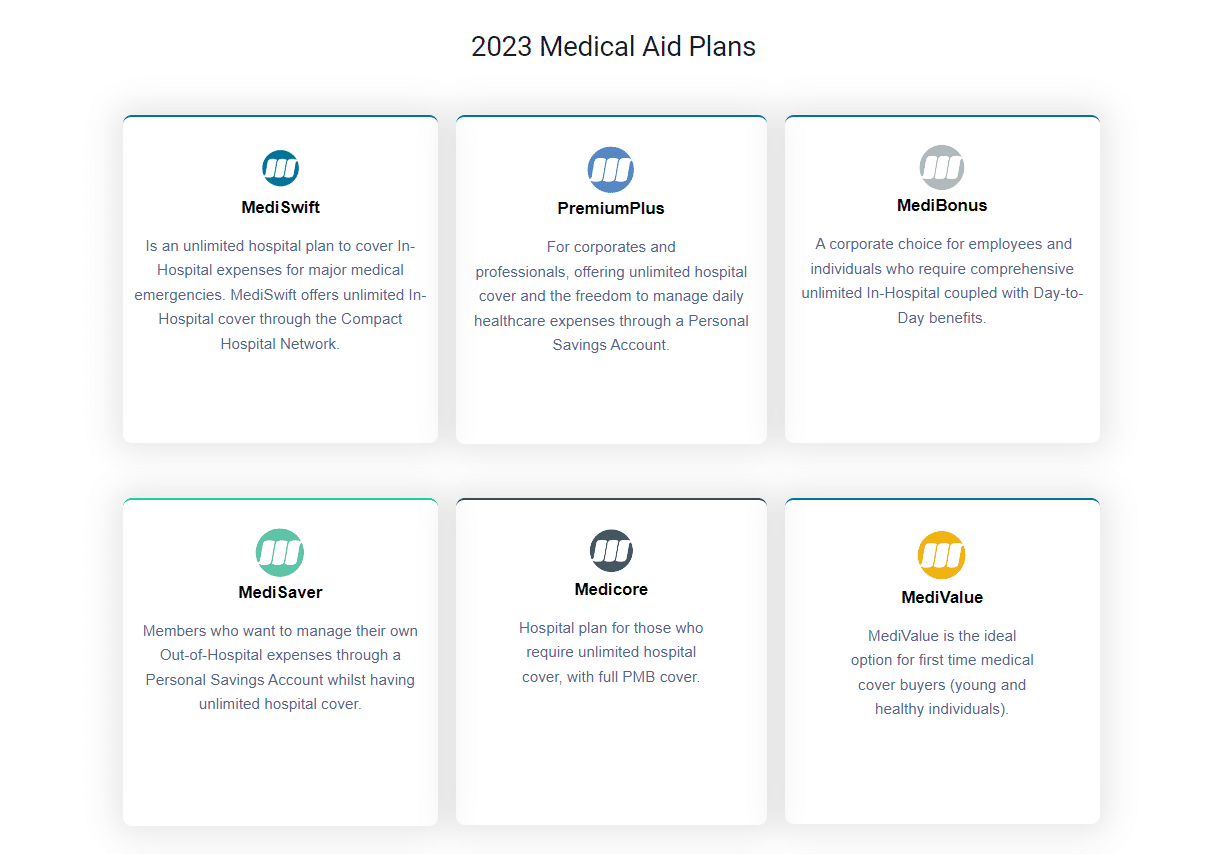
MedShield has the following medical aid plans to offer:
- ✅ MedShield MediCurve
- ✅ MedShield PremiumPlus
- ✅ MedShield MediValue Prime
- ✅ MedShield Value Compact
- ✅ MedShield MediSwift
- ✅ MedShield MediSaver
- ✅ MedShield MediPlus Prime
- ✅ MedShield MediPlus Compact
- ✅ MedShield MediPhila
- ✅ MedShield MediCore
- ✅ MedShield MediBonus
Medshield MediBonus Plan Contributions
| 👤 Main Member | 👥 +1 Adult Dependent | 🍼 +1 Child Dependent |
| R7,587 | R5,328 | R1,578 |
Discover the 5 Best Medical Aids under R500
Medshield MediBonus Plan Benefits and Cover Comprehensive Breakdown
MediBonus Hospital-At-Home
- Medshield offers a Hospital-at-Home service delivered by Quro Medical.
- The Hospital-at-Home service offers an alternative to hospitals as the center of patient care and management.
- Hospital-at-Home provides active treatment at home instead of a general hospital ward for a specified period without compromising the quality of care.
- Patients more vulnerable to hospital-acquired infections and developing new health complications may benefit from care at home.
- Patients who usually need admission to a general hospital ward are eligible for Hospital-at-Home.
- Quro Medical works with each patient and their treating doctor to develop a personalized treatment plan to deliver at home.
- Treatment plans are amended accordingly if a patient’s medical needs change during treatment.
- The clinical team at Quro Medical arranges routine home visits customized to the individual’s specific needs that may occur daily or more frequently to provide the necessary treatment and care.
- Other channels allow patients to access advice and support outside of home visits.
MediBonus Major Medical Benefits In-Hospital
| 📌 Overall Annual Limit | There is no overall annual limit. |
| 📍 Extended Benefit Cover of up to 200% | This only applies to specific services and procedures in hospitals. |
| 🚑 Hospitalization | Unlimited cover. Subject to the relevant Management Healthcare Program. Pre-approval is needed for specialist services. Specialist visits and consults must be pre-authorized. |
| ➡️ Surgical Procedures | Covered as part of an authorized event. Unlimited cover provided. Extended Benefit Cover of up to 200%. |
| 💊 Medicine upon discharge | Limited to R830 per admission. Per the Maximum Generic Pricing of Medicine Price List and Medshield Formulary. |
| 🔁 Hospitalisation Alternatives Physical Rehabilitation Sub-Acute Facilities Nursing Services Hospice Terminal Care | Clinical Protocols will apply. There is an R98,780 limit per family yearly, subject to the hospitalization limit. DSPs must be used, or a 25% co-payment will apply for using a non-MediBonus Network Hospital. Terminal care is limited to R41,400 per family per year and is subject to the Alternatives to Hospitalisation Limit. |
| 🩺 General, Medical, and Surgical Appliances | Limited to R15,760 per family per year. Pre-approval is required. Services must be obtained from a DSP, Network Provider, or Preferred Provider. |
| ☑️ Hiring or buying of Appliances, External Accessories, or Orthotics | Limits Apply |
| ✅ Peak Flow Meters, Nebulizers, Glucometers, and Blood Pressure Monitors (needs motivation) | Limited to R885 per beneficiary yearly. Subject to the Appliance Limit |
| 🦻 Hearing Aids (including repairs) | Subject to the Appliance Limit |
| 👩🏻🦼 Wheelchairs (including repairs) | Subject to the Appliance Limit |
| ✔️ Stoma Products and Incontinence Sheets relating to Stoma Therapy | Unlimited if pre-approved. |
| 😴 CPAP Apparatus for Sleep Apnea | Subject to the Appliance Limit |
| ➡️ Oxygen Therapy Equipment | Unlimited cover. Subject to pre-authorization and the relevant Managed Healthcare Program. Clinical Protocols will apply. |
| 📈 Home Ventilators | Unlimited cover. Subject to pre-authorization and the relevant Managed Healthcare Program. Clinical Protocols will apply. |
| 🩸 Blood, Blood Equivalents, and Blood Products | Unlimited cover. Subject to pre-authorization and the relevant Managed Healthcare Program. Clinical Protocols will apply. |
| 👨⚕️ Medical Practitioner Consultations and Visits during hospital admission | Unlimited cover. Forms part of an authorized event during hospitalization and includes Medical and Dental Specialists or FPs. Extended Benefit cover of up to 200%. |
| 🤓 Refractive Surgery Includes the following: LASIK Radial Keratotomy Phakic Lens Insertion | Limited to R19,760 per family per year. The benefit includes hospitalization. Without pre-authorization, the account will be settled from daily benefits limits. Subject to pre-authorization by the relevant Managed Healthcare Program. Services must be obtained from the Medshield Hospital Network, and the Medshield Specialist Network might be required. |
| 💤 Sleep Studies Diagnostic Polysomnograms | Unlimited Cover Subject to pre-authorization by the relevant managed healthcare program. Clinical protocols will apply. |
| ✳️ CPAP Titration | Unlimited cover. Subject to pre-authorization by the relevant managed healthcare program. Clinical protocols will apply. |
| ❤️ Organ, Tissue, and Haemopoietic Stem Cell (Bone Marrow) Transplants Immuno-Suppressive Medication Post Transplantation biopsies and scans. Related radiology and pathology | Subject to the relevant managed healthcare program. 25% upfront co-payment for the use of a non-Medshield Network Hospital. Organ harvesting is limited to the Republic of South Africa. Workup costs for the donor in Solid Organ Transplants are included. No benefits for international donor search costs. Hemopoietic stem cell (bone marrow) transplantation is limited to allogenic grafts and autologous grafts derived from the South African Bone Marrow Registry. |
| 🌎 International Corneal Grafts and Transplants | Limited to R46,615 per beneficiary. Subject to the OAL. Clinical protocols apply. |
| 🚩 Local Corneal Grafts and Transplants | Limited to R19,980 per beneficiary. Subject to the OAL. Clinical protocols apply. |
| ⚕️ Pathology and Medical Technology | Unlimited cover. Clinical protocols apply. Must be part of an authorized event but excludes allergy and Vitamin D testing. |
| 🦵 Physiotherapy | Limited to R2,955 per beneficiary yearly. Once this is exhausted, the benefit is subject to the day-to-day limit unless specific authorization is obtained. |
| 🦾 Internal Prostheses and Devices | Subject to pre-authorization by the relevant Managed Healthcare Program. Only for surgically implanted devices. Limited to R53,280 per family yearly. 25% co-payment unless related to PMB. Hips and knees sub-limit: R35,510 per beneficiary. |
| 🔍 External Prostheses | Must be pre-approved. Treatment can only be obtained from a DSP, Network Provider, or Preferred provider. The benefit includes Ocular Prostheses. Clinical protocols apply. Subject to prostheses and the device’s internal limit. There are no co-payments on external prostheses. |
| 📍 Long Leg Callipers | Subject to prostheses and the device’s internal limit. There are no co-payments on external prostheses. |
| 1️⃣ Basic Radiology | Unlimited cover. Clinical protocols will apply. |
| 2️⃣ Specialized Radiology | Limited to R24,750 per family yearly for in- and out-of-hospital. Subject to pre-authorization by the Managed Healthcare Program. Services must be obtained from the Medshield DSP or Network Provider. |
| 3️⃣ CT Scans, MUGA Scans, MRI Scans, Radio Isotope Studies | Subject to the Specialised Radiology Limit. Clinical protocols will apply. |
| 4️⃣ CT Colonography (Virtual colonoscopy) | There is no co-payment on this benefit. Clinical protocols apply. |
| 5️⃣ Interventional Radiology replacing Surgical Procedures | Unlimited cover, but clinical protocols apply. |
| ❤️ Chronic Renal Dialysis Hemodialysis and Peritoneal Dialysis include the following: Material Medication Related Radiology and Pathology | Unlimited cover. A non-DSP will incur a 35% upfront co-payment. Use of a DSP with Rand one for PMB and non-PMB. |
| 🧡 Non-Surgical Procedures and Tests | Unlimited cover. It must be as part of an authorized event. Members must use the Medshield Specialist Network. |
| 🧠 Mental Health | Limited to R45,790 per family per year in and out-of-hospital. 25% upfront co-payment for non-Medshield Network Hospitals. DSP from Rand one applies for PMB and non-PMB admissions. |
| 💜 Rehabilitation for Substance Abuse | Subject to the mental health limit. |
| 👩⚕️ Consultations and Visits, Procedures, Assessments, Therapy, Treatment, or Counselling | Subject to the mental health limit. |
| 😷 HIV and Aids | According to the Managed Healthcare Protocols. Pre-authorization and Managed Healthcare Program registration are required. |
| 💉 Anti-retroviral and related medicines | Voluntary out-of-formulary or PMB medication from a non-DSP supplier requires a 35% upfront co-payment. |
| 💊 HIV/AIDS-related Pathology and Consultations | Voluntary out-of-formulary or PMB medication from a non-DSP supplier requires a 35% upfront co-payment. |
| 📌 National HIV Counselling and Testing (HCT) | Voluntary out-of-formulary or PMB medication from a non-DSP supplier requires a 35% upfront co-payment. |
| 📍 Infertility Interventions and Investigations | Clinical Protocols apply. Limited to interventions and investigations only. Pre-authorization and Managed Healthcare Program registration are required. |
POLL: 5 Best Hospital Plans under R1500 in South Africa
MediBonus Oncology Benefits
| 📌 Oncology Limit | Limited to R552,925 per family per year. There is a 40% co-payment if members use a non-DSP. |
| 📍 Active Treatment (Includes Stoma Therapy, Incontinence Therapy, and Brachytherapy) | Subject to the Oncology Limit. ICON Standard Protocols apply. |
| ☑️ Oncology Medicine | Subject to the Oncology Limit. ICON Standard Protocols apply. |
| ✅ Radiology and Pathology | Subject to the Oncology Limit. |
| ✳️ PET and PET-CT | Limited to 2 scans per family per annum. Subject to the Oncology Limit. |
| 💗 Integrated Continuous Cancer Care | Six visits per family per annum. Subject to the Oncology Limit |
| 💊 Specialized Drugs for Oncology, Non-Oncology, and Biological Drugs | Limited to R223,520 per family yearly. Subject to the Oncology medicine limit. Pre-authorization is required from the Oncology Managed Healthcare provider. Clinical Protocols will apply. 20% upfront payment for non-PMBs. |
| ➡️ Vitreoretinal Benefit | Subject to pre-approval. Specialized Drugs Limit applies. |
| ⚕️ Breast Reconstruction (only after an oncology event) | Subject to pre-authorization. Clinical protocols apply. The benefit is only for Post Mastectomy (all stages) Services must be obtained from a DSP network or provider. Member must use the Medshield Specialist Network. Limited to R94,105 per family yearly and limited to (and included) in the hospitalization limit. Co-payments and prostheses limits will not apply for Breast Reconstruction. |
MediBonus Chronic Medicine Benefits
Members must use a DSP Provider on MediBonus
- Limited to R16,490 per beneficiary and R32,980 per family per year.
- Medications will be approved per the Medshield Formulary and will be available beginning with Phase one.
Supply of Medication (One month in advance)
- Limited to R16,490 per beneficiary and R32,980 per family per year.
- Medications will be approved per the Medshield Formulary and will be available beginning with Phase one.
MediBonus Chronic Disease List
Medshield MediBonus covers 26 CDL conditions plus an additional 44, including:
- ☑️ Addison’s disease
- ☑️ Asthma
- ☑️ Bi-Polar Mood Disorder
- ☑️ Bronchiectasis
- ☑️ Cardiac failure
- ☑️ Cardiomyopathy
- ☑️ Chronic renal disease
- ☑️ Chronic obstructive pulmonary disease
- ☑️ Coronary artery disease
- ☑️ Crohn’s disease
Discover the 5 Best Medical Aids for Chronic Illness Cover
MediBonus Dentistry Benefits
| 🦷 Basic Dentistry: In-Hospital | Unlimited cover provided. The in-hospital cover is only for kids under 6 for comprehensive Basic Dental). Subject to Managed Healthcare Program pre-authorization. Treatment without authorization incurs a 20% penalty. MediBonus members must use the Medshield Hospital Network. |
| 🪥 Basic Dentistry: Out-of-Hospital | Unlimited cover provided. According to the Dental Managed Healthcare Program, protocols. Members must use the Medshield Dental Network. Pre-authorization is required for plastic dentures. A 20% penalty will be imposed if permission is not obtained before treatment. |
| 📌 Specialized Dentistry | There is a limit of R19,380 per family yearly. All services are subject to pre-approval by the applicable Managed Healthcare Program. A 20% penalty will be imposed if permission is not obtained before treatment. Protocols and the Medshield Dental Network apply according to the Dental Managed Healthcare Program. |
| 📍 Impacted Teeth, Wisdom Teeth, and Apicectomy Only hospitalization, general anesthetics, or conscious sedation for bone impactions. Practitioners only cover out-of-hospital apicectomy of permanent teeth. Pre-authorization and Hospital Managed Healthcare Programs apply. Dental Managed Healthcare Programs, Protocols, and Medshield Dental Network apply. Pre-authorization for general anesthesia and conscious sedation pre-authorization, in- and out-of-hospital. No authorization is needed for local anesthetic apicectomy, impacted tooth removal, or wisdom tooth removal. | The Specialist Dentistry Restriction applies. An R900 co-payment is required for wisdom teeth extraction in a Day Clinic. An upfront co-payment of R2,000 is required if the procedure is performed in-hospital. There is no co-payment if the procedure is performed under conscious sedation in the Practitioners’ rooms. |
| ☑️ Dental Implants Covers implant-related services. Must be pre-approved. The Dental Managed Healthcare Programme, Protocols, and Medshield Dental Network apply. | The Specialist Dentistry Limit applies. |
| ✅ Orthodontic Treatment Pre-approval is required. Protocols and the Medshield Dental Network apply according to the Dental Managed Healthcare Program. | The Specialist Dentistry Limit applies. |
| 👑 Crowns, Bridges, Inlays, Mounted Study Models, Partial Chrome Cobalt Frame Base Dentures, and Periodontics Includes consultations, visits, and treatment for all types of dentistry, including technician fees. Pre-approval is required. Protocols and the Medshield Dental Network apply according to the Dental Managed Healthcare Program. | The Specialist Dentistry Limit applies. |
| 😊 Maxillo-facial Surgery | Limited to R20,870 per family yearly. Extended benefit cover of up to R200%. Subject to pre-approval. The benefit is only for non-elective surgery. Subject to the Dental Management Healthcare Program and Protocols. Must use a provider from the Medshield Hospital Network. It might be subject to using the Medshield specialist network. |
You might also like this poll: Best Medical Aids in South Africa Covering Braces
MediBonus Maternity Benefits
There will be benefits during pregnancy, after birth, and following delivery. However, pre-authorization with the applicable Managed Healthcare Program is required before hospital admission. Unless otherwise specified, benefits are allocated for each pregnancy subject to the Total Yearly Limit. A complimentary baby bag from Medshield can be obtained during the third trimester.
Ladies can make use of our free Ovulation Calculator
| 🍼 Antenatal Consultations | Twelve Consultations per pregnancy. It might be subject to the use of the Medshield Specialist Network. |
| 👶 Antenatal Classes and Postnatal Midwife Consults | Eight Visits per event. |
| 📈 Scans | Two 2D scans per pregnancy. |
| 📉 Amniocentesis Tests | One per pregnancy |
| 🏥 Confinement In-Hospital | Unlimited cover. Extended benefit cover of up to 200%. |
| 👨⚕️ Delivery by a Family Practitioner or Medical Specialist | Unlimited cover. |
| 💙 Confinement in a registered birthing unit or out-of-hospital | Unlimited cover Must use a Medshield Network. |
| 👩⚕️ Delivery by a registered Midwife or a Practitioner | Covered up to 200% of the Medshield Private rates (only for a registered Midwife). |
| 🔍 Hire a water bath and oxygen cylinder | Unlimited cover. |
You might like Medical Insurance for Pregnancy

Medshield MOM Program and Benefits
To support women on their journey to motherhood, Medshield MOM has launched a dedicated website that provides information and resources for all stages of pregnancy, birth, and postpartum. This website is an easily accessible hub of valuable health, fitness, nutrition, motherhood, babies, toddlers, and more content tailored to the pre-and post-partum phases. As a Medshield member, you can take advantage of the pregnancy-related benefits. The Medshield MOM website will ensure you are fully informed of your options.
Some of the features and advantages include, but are not limited to, the following:
- A guide for your journey from start to finish.
- Convenient, dependable, and easily accessible pregnancy resources.
- A toddler benefit that includes information on child immunization, child nutrition, a nurse helpline available 24/7, and digital/online kid yoga.
- Advice formulated by professionals.
- Reminders through email to arrange doctor’s appointments and request hospital pre-authorizations, etc.
- Emails containing updates on your unborn child’s growth and development.
- Mothers can register and enter the specific week of their pregnancy journey. Then, they will begin getting content based on that time and continuing ahead.
- The Medshield MOM bags are made locally utilizing recyclable, eco-friendly materials. These distinctive bags are filled with excellent Bennetts products for your child.
MediBonus SmartCare Services and Benefits
SmartCare gives access to Videomed and telephone plus video consultations through a select group of healthcare professionals. SmartCare is a developing healthcare benefit aiming to provide members with convenient care access. SmartCare services include the following Acute and Chronic consultations.
| 1️⃣ Pharmacy/clinic private nurse practitioner consultations | Unlimited cover. |
| 2️⃣ Nurse-led Videomed family practitioner (FP) consultations | One visit per family is subject to the Overall Yearly Limit, followed by the Family Practitioner (FP) Consultations and Visits Limit. |
| 3️⃣ WhatsApp doc advice line | Unlimited cover. |
MediBonus Day-to-Day Benefits
| 📌 Day-to-Day Limit | The following limits apply: Main Member – R12,000 Main Member + 1 Dependent – R17,990 Main Member + 2 Dependents – R19,980 Main Member + 3 Dependents – R21,975 Main Member + 4> Dependents – R23,760 |
| 📍 Family Practitioner (FP) Consultations and Visits Out-of-Hospital | Subject to the day-to-day limit. |
| ☑️ Medshield Family Practitioner Network (Consults and Visits out-of-hospital) | Two visits per beneficiary, according to the OAL. |
| ✅ Extended FP visits for emergency and chronic FP consultations (In-person only) | Registration in the Disease Management Program is required. Pre-approval is needed. Chronic Disease List and Clinical Protocols Apply. Once the Day-to-Day Limit and Care Plan FP visits have been depleted, visits are unlimited. There is a limit of one FP consultation per beneficiary. |
| 👩⚕️ Medical Specialist Consultations and Visits | Must use the Medshield Specialist Network. Subject to the day-to-day limit. |
| 🚑 Casualty and emergency visits | Subject to the day-to-day limit. |
| 💊 Acute Medicine | Subject to the day-to-day limit. |
| ➡️ Pharmacy Advised Therapy (PAT) | Subject to the day-to-day limit. Limited to R250 per script and one script per beneficiary daily. |
| 🤓 Optometry | Subject to one pair of Optical Lenses and a frame or Contact lenses per beneficiary every 2 years. The Optical Service Date Cycle will determine the extent of this benefit. Subject to the OAL. |
| 👓 Optometric Refraction Eye Tests | One test per beneficiary per 24-month optical cycle. Subject to the OAL. Subject to the Optical Limit. |
| 📈 Spectacles or Contact Lenses | Subject to the Optical Limit. |
| 📉 Frame or lens enhancement | Limited to R1,165 per beneficiary. Limited to (and included in) the Optical Limit. |
| 📊 Reading Glasses | There is a limit of R190 per beneficiary. Subject to the OAL. Must be supplied by a registered Optometrist, Ophthalmologist, Supplementary Optical Practitioner, or a registered Pharmacy. |
| ➡️ Pathology and Medical Technology | Subject to the Day-to-Day Limit. Subject to the relevant Pathology Managed Healthcare program and protocols. |
| 😷 Covid-19 PCR/Antigen Test | The 1st test is included in the OAL, and subsequent tests provide no benefit unless the result is positive and subject to PMB. |
| ☑️ Physiotherapy, Biokinetics, and chiropractics | Subject to the Day-to-Day Limit. |
| ✅ Basic Radiology | Subject to the Day-to-Day Limit. There is a limit of one bone densitometry scan per beneficiary yearly in or out-of-hospital. Subject to the Radiology Managed Healthcare Program and Protocols. Subject to the Medshield Basic Radiology formulary. |
| 📌 Specialized Radiology | Limited to R24,750 In- and Out-of-Hospital, per family yearly. Limited to (and included in) the Specialised Radiology Limit. Subject to pre-authorization by the relevant Managed Healthcare Program |
| 📍 Non-Surgical Procedures | Subject to the Day-to-Day Limit. |
| ☑️ Procedures and Tests performed in the Practitioner’s rooms | Unlimited cover. Medshield Private Rate covers up to 200%. |
| ✅ Routine diagnostic Endoscopic Procedures performed in the Practitioner’s rooms | If done in practitioner’s rooms, it is limited to and included in the overall annual limit. Medshield Private Rate covers up to 200%. In-Hospital co-payment is not required for children aged 8 and under. |
| 🧠 Mental Health Includes the following: Consultations and Visits Procedures Assessments Therapy Treatment or Counselling | Limited to R5,550 per family yearly. Limited to (and included in) the day-to-day limit of R45,790. |
| ⚕️ Intrauterine Devices and Alternatives | Covers consultation, pelvic ultrasound, sterile tray, device, and insertion, if performed the same day. Subject to the applicable clinical protocols. The Medshield Specialist Network must be utilized. It should be performed at the practitioner’s office. Only covered if no hormonal contraceptives are taken, but only upon application Limited to 1 per female recipient. Subject to the Yearly Maximum Limit. Included are all IUD brands up to the cost of the Mirena device. One Mirena/Kyleena device per female patient every five years. Implanon – one per female recipient every three years. One Nova T/Copper device per female patient every two years. |
| 🩺 Additional Medical Services Including the following: Audiology Genetic Counselling Hearing Aid Acoustics Occupational Therapy Orthoptics Podiatry Speech Therapy and Private Nurse Practitioners Dietetics | The in-hospital referral is subject to authorization. Subject to the Day-to-Day Limit. |
| 🧪 Alternative Healthcare Service (Only applies to Acupuncturists, Homeopaths, Naturopaths, Osteopaths, and Phytotherapists) | Subject to the Day-to-Day Limit. |
MediBonus Wellness Benefits
Medshield’s Wellness Benefit program empowers members to proactively manage their health by undergoing preventative tests and procedures. The company strongly advises its members to schedule the necessary tests at least once per year. Medshield members must use pharmacies included in their benefit options’ Pharmacy Network to access the Wellness Benefits. Members must note that benefits are subject to the Overall Annual Limit. Once that limit has been reached, the benefits will be subject to the Day-to-Day limit. However, consultations for specific services are excluded from these limits.
| 💉 Adult Vaccination | Limited to R1,795 per family per annum. After the limit is reached, it is taken from the daily benefit. |
| 💊 Birth Control (Contraceptive Medicine) | Limited to a maximum of 13 prescriptions per year per female recipient between the ages of 14 and 55, with an R200 limit per prescription. Subject to Acute Medical Benefit Limit. Only relevant in the absence of intrauterine devices and alternatives. |
| 🦵 Bone Density Testing for Osteoporosis and bone fragmentation | One per beneficiary 50 years> every three years. |
| 😷 COVID-19 Vaccines | Subject to the Overall Annual Limit. Protocols apply. |
| 📌 Flu Vaccines | One per beneficiary aged 18 or older is included in the Yearly limit. After that, it is paid from the daily benefit. |
| 📍 Pap Smear | One per female beneficiary. |
| 📈 Health Risk Assessment on the SmartCare Network Cholesterol Blood Glucose Blood Pressure Body Mass Index (BMI) | One per beneficiary 18> |
| 📉 Pneumococcal Vaccination | One per annum for high-risk individuals and beneficiaries 60 years>. |
| 📊 National HIV Counselling Testing (HCT) | One test per beneficiary. |
| 📌 HPV Vaccination | One course of two injections per female beneficiary between 9 to 13 years old. Subject to qualifying criteria. |
| 📍 Mammogram (Breast Screening) | One per female beneficiary 40 years> every 2 years. |
| ☑️ PSA Screening for male beneficiaries | Subject to the day-to-day limit. |
| ✅ Tuberculosis Test | One test per beneficiary. |
Wellness Benefits – Child Immunisations
This benefit and immunization program as per the Department of Health Protocols according to these age groups:
| 🍼 At Birth | Tuberculosis (BCG) Polio OPV |
| 👶 6 Weeks | Polio (OPV) Diphtheria Tetanus, Pertussis (Whooping Cough) Hepatitis B Hemophilus Influenza B (HIB) Rotavirus Pneumococcal |
| 📌 10 Weeks | Polio, Diphtheria, Tetanus, Pertussis (Whooping Cough) Hepatitis B Hemophilus Influenza B (HIB) Pneumococcal Rotavirus (Optional |
| 📍 14 Weeks | Polio Diphtheria Tetanus Pertussis (Whooping Cough) Hepatitis B Hemophilus Influenza B (HIB) Rotavirus Pneumococcal |
| ❤️ 6 Months | Measles MV (1) |
| 🧡 9 Months | Measles, Pneumococcal, and Chickenpox CP |
| 💛 12 Months | Measles MV (2) |
| 💚 15 Months | Chickenpox CP |
| 💙 18 Months | Polio, Diphtheria, Tetanus, Pertussis (Whooping Cough) Measles Mumps and Rubella (MMR) |
| 6️⃣ 6 Years | Polio Diphtheria and Tetanus (DT) |
MediBonus Prescribed Minimum Benefits
Medshield members are entitled to cover Prescribed Minimum Benefits (PMBs), regardless of their chosen benefit option. Medshield assumes the cost of PMB treatments if they are provided by one of Medshield’s Designated Service Providers (DSPs) in compliance with the Scheme Rules.
The Medical Schemes Act 131 of 1998 mandates that all medical plans must cover the costs associated with the following:
- Any potentially fatal medical emergency.
- A set of 26 Chronic Disease List (CDL) diseases that are well-defined.
- 271 DTP diagnoses.
In-Hospital Admissions for treating PMBs:
- If you are diagnosed with a PMB disease requiring hospitalization, you must comply with the Medshield hospital authorization process.
- It would help if you utilized a hospital that is a part of the Hospital Network for your selected insurance package, as all stay, and treatment fees have negotiated prices.
- Specialist services obtained during hospitalization are reimbursed at the Scheme rate.
- If the Scheme rate does not cover the entire claim amount, you must apply to the Scheme and request that the Specialist’s rate be paid at cost instead of the Scheme rate.
Out-of-Hospital treatment and managing PMBs:
- Members diagnosed with any 26 CDL conditions covered by Medshield and MediBonus must apply to Mediscor for approval.
- The member automatically receives a Care Plan (treatment plan) notification from the Scheme after the healthcare provider claims with the ICD-code as authorized.
- The Care Plan details and approves benefits like radiography, pathology, and doctors’ visits.
- After using the Care Plan, the member and their treating provider must fill out a PMB Application form to seek clearance for further treatment.
- If approved, a revised Care Plan will include the additional treatment.
MediBonus Option Payment for PMB conditions:
- While the funds in members’ PMSA come directly from the members themselves, the Risk Pool is responsible for covering the expenses associated with the care outlined in the members’ Care Plans (OAL).
- The Member may request that the Scheme reprocess claims for services previously paid for by the Member but are included in the Care Plan.
- It should be emphasized that this only pertains to the services included in the finalized Care Plan.
271 DTP Conditions:
- Members with DTP must complete a PMB application form with their doctor.
- If they do not complete a PMB Application form, the Day-to-Day Savings will pay for treatment.
- The Care Plan (treatment plan) will list the covered treatments for the condition after clinical assessment and approval.
COVID-19 as a PMB
- Respiratory DTP PMB includes Covid-19.
- After seeing a doctor, members might need a COVID-19 PCR or SARS-CoV-2 Antigen test.
- According to the Plan Regulations, this benefit requires a doctor or nurse referral and payment.
- MediBonus covers either a PCR or an antigen test, but not both.
MediBonus COVID-19 Benefits and Access to Care
COVID-19 PCR Test or Antigen Tests
The COVID-19 PCR Test or Antigen Tests have the following features and conditions:
- The First COVID PCR or antigen test is covered in the Overall Annual Limit (OAL).
- Depending on the option, the Second and subsequent tests are covered by daily limits or a medical savings plan. If these benefits are not available, members must pay for the tests.
- The 2nd and subsequent positive PCR or Antigen tests are covered first from Day-to-Day benefit or Savings, then from OAL if PMB applies.
- The pathology test will be reimbursed as a PMB by Risk after emailing the positive results to Medshield. Risk
- Benefits require a PMB Application form, and Clinical Protocols apply.
- Travel and non-symptomatic COVID-19 tests are excluded from this benefit.
- Scheme risk gives members the Day-to-Day restriction. Therefore, PMB COVID-19 treatment will pay from a Day-to-Day benefit until it is gone and then from Risk (OAL).
MediBonus Plan Exclusions and Waiting Periods
MediBonus Exclusions
MediBonus does not cover some of the following:
- Cosmetic crown and bridge procedures, as well as the accompanying laboratory fees
- Crown and bridge procedures with minimal tooth structural loss and accompanying laboratory costs
- Rehabilitation of the occlusion and the related laboratory expenditures
- Provisional crowns, as well as the accompanying laboratory fees
- Emergency crowns that are not inserted immediately to safeguard a tooth after an injury, as well as the related laboratory expenditures
- Gold, precious metal, semi-precious metal, and platinum foil prices
- Fees for laboratory delivery
- Unless expressly authorized and unless PMB level of care, orthopedic shoes, and boots
- TENS and APS pain relief machines
- Stethoscopes
- Procedures for sinus lift
- When claimed in conjunction with impacted teeth, closing an oral-antral opening
- Orthognathic (jaw correction) surgery, as well as any associated hospital expenditures and laboratory fees
- Aortic stents are covered until the Prescribed Minimum Benefits level of care (DSP) is met
- Peripheral vascular stents are covered unless the Prescribed Minimum Benefits level of care (DSP) is met
- Mineral trioxide cost
- Enamel micro-abrasion
- Dental procedures or equipment that is not deemed clinically necessary or desirable by the applicable Managed Healthcare Program
MediBonus Waiting Periods
Often, there is a waiting period for pre-existing conditions. This is to prevent new members from abusing medical insurance for a brief period to finance pricey procedures and cancel their membership shortly after. According to the Medical Schemes Act No. 131 of 1998, the following waiting periods may apply:
- A 3 (three) month general waiting time for all benefits.
- A maximum 12 (twelve) month exclusion for a previous ailment.
- A late joiner contribution penalty.
Medshield MediBonus Plan vs. Similar Plans from other Medical Schemes
| 🔎 Medical Aid | 🥇 Medshield MediBonus | 🥈 Profmed ProSecure Savvy | 🥉 Momentum Extender |
| 👤 Main Member Contribution | R7,587 | R | R6,589 |
| 👥 Adult Dependent Contribution | R5,328 | R | R4,997 |
| 🍼 Child Dependent Contribution | R1,578 | R | R1,937 |
| 🌎 International Cover | Only Organ Transplants | R8 million | R9.01 million |
| 🚑 Hospital Cover | Unlimited | Covers up to 100% of the negotiated tariff | Unlimited |
| 💶 Prescribed Minimum Benefits | ☑️ Yes | ☑️ Yes | ☑️ Yes |
| 📉 Screening and Prevention | ☑️ Yes | ☑️ Yes | ☑️ Yes |
| ➡️ Oncology Cover | R552,925 | R466,155 | R500,000 |
| 💙 Maternity Benefits | ☑️ Yes | ☑️ Yes | ☑️ Yes |
Our Verdict on The MediBonus Plan
Medshield MediBonus is a comprehensive health insurance plan designed to cater to the healthcare needs of individuals and families. The plan offers a range of benefits, including unlimited private hospital coverage, chronic medication, and day-to-day medical expenses. MediBonus plan members have access to a broad network of healthcare providers and facilities, ensuring they receive quality medical care when needed. One of the significant advantages of the MediBonus plan is its unlimited hospital cover, which means that members do not have to worry about running out of funds during a hospital stay. The plan also covers the cost of chronic medication for 27 specified chronic conditions and an additional 44, ensuring that members receive the necessary treatment for their long-term health conditions.
MediBonus also covers day-to-day medical expenses, such as GP consultations, blood tests, X-rays, and medication. One of the drawbacks of the MediBonus plan is that it may not be suitable for individuals who do not require comprehensive medical coverage. The plan’s premium is higher than other plans offered by Medshield, making it less affordable for some individuals. Additionally, the plan does not cover some medical procedures available in other plans offered by Medshield. Compared to other plans offered by Medshield, the MediBonus plan offers more comprehensive medical coverage.
However, this also means it comes with a higher premium, making it less affordable for some individuals. For instance, the Medshield MediCore Plus plan offers more affordable premiums. Still, it covers hospitalization, chronic medication, and day-to-day medical expenses. However, it does not offer the same level of medical coverage as the MediBonus plan.
You might also like the following plans MedShield has to offer:
- ✅ MedShield MediCurve
- ✅ MedShield PremiumPlus
- ✅ MedShield MediValue Prime
- ✅ MedShield Value Compact
- ✅ MedShield MediSwift
- ✅ MedShield MediSaver
- ✅ MedShield MediPlus Prime
- ✅ MedShield MediPlus Compact
- ✅ MedShield MediPhila
- ✅ MedShield MediCore
MediBonus Plan Frequently Asked Questions
What is Medshield MediBonus, and how does it work?
Medshield MediBonus is a comprehensive medical aid plan offered by Medshield Medical Scheme in South Africa. The plan provides members with cover for private hospitalization, chronic medication, and day-to-day medical expenses. Furthermore, members can access a network of healthcare providers and facilities, ensuring they receive quality medical care. The plan’s premium is based on the member’s income and the number of dependents covered.
What is covered under the Medshield MediBonus plan?
The MediBonus plan covers unlimited private hospitalization, chronic medication for 27 specified chronic conditions and an additional 44 conditions, and day-to-day medical expenses, such as GP consultations, blood tests, X-rays, and medication. In addition, the Medshield MediBonus plan also covers up to 200% of the extended cover benefit for specific treatments.
How much does the Medshield MediBonus plan cost?
MediBonus is R6,966 for the primary member, R4,893 per adult dependent, and R1,499 per child dependent. However, the plan’s premium is higher than other plans offered by Medshield, making it less affordable for some individuals.
What are the advantages of the Medshield MediBonus plan?
One of the significant advantages of the MediBonus plan is its comprehensive medical cover, which includes unlimited hospital cover, chronic medication, and day-to-day medical expenses. The plan provides members access to a network of healthcare providers and facilities, ensuring that they receive quality medical care no matter where they are in South Africa.
Are there any drawbacks to the Medshield MediBonus plan?
One of the drawbacks of the MediBonus plan is that it may not be suitable for individuals who do not require more affordable medical coverage. The plan’s premium is higher than other plans offered by Medshield, making it less affordable for some individuals. Additionally, the plan does not cover some medical procedures available in other plans offered by Medshield.
What other medical aid plans does Medshield offer?
Medshield offers a range of medical aid plans to cater to different healthcare needs and budgets. These plans include MediCore, MediSaver, MediValue, and MediPlus. Each plan has its own unique benefits and features, allowing members to choose the one that best suits their needs and budget.
You might also like
Table of Contents
Free Medical Aid Quote
Our Trusted Partners
We work with leading medical aid companies in South Africa.

7 Actionable Ways to save 32% on your MEDICAL AID in 14 days.

- +27 72 7967 530
- [email protected]
- 2nd Floor, West Tower, Nelson Mandela Square, Sandton, 2196, Johannesburg, Gauteng, South Africa
🔎 Report a bug or outdated data to be updated to [email protected]
© Medicalaid.com | All rights Reserved |
Copyright 2024
Top 5 Medical Aids
Top 5 Gap Cover Plans
































